Exam Code: CDIP
Exam Name: Certified Documentation Integrity Practitioner
Certification Provider: AHIMA
Corresponding Certification: CDIP
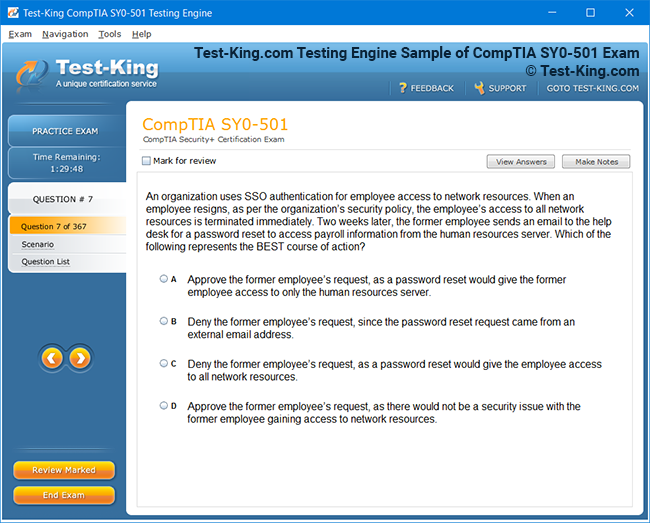
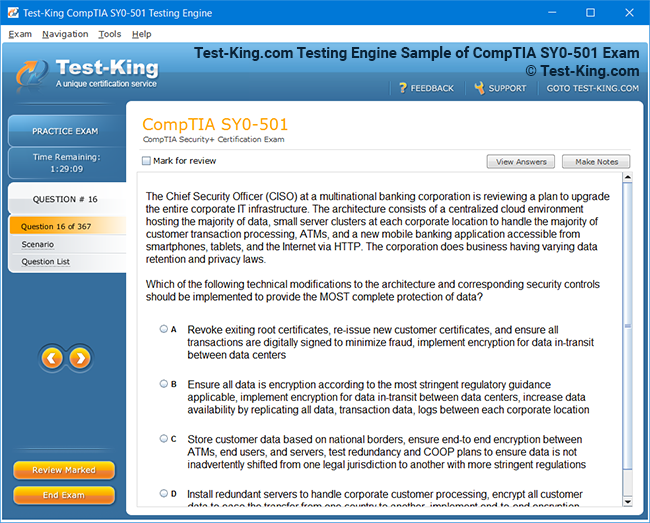
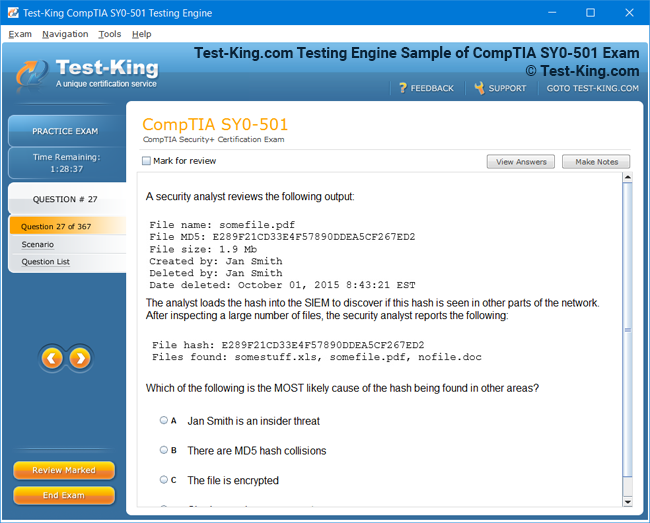
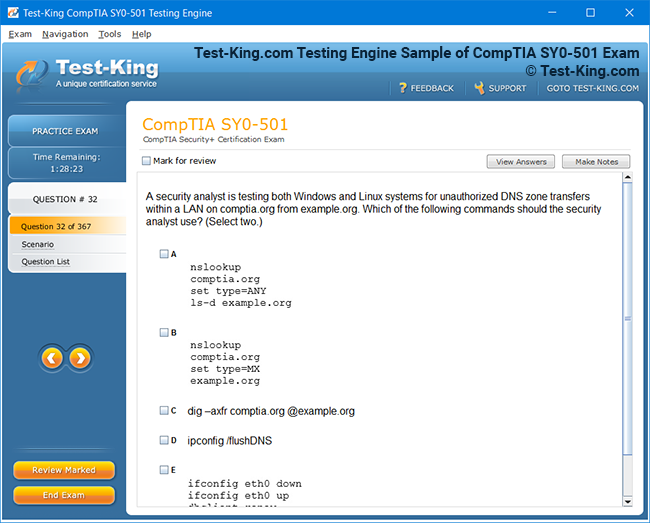
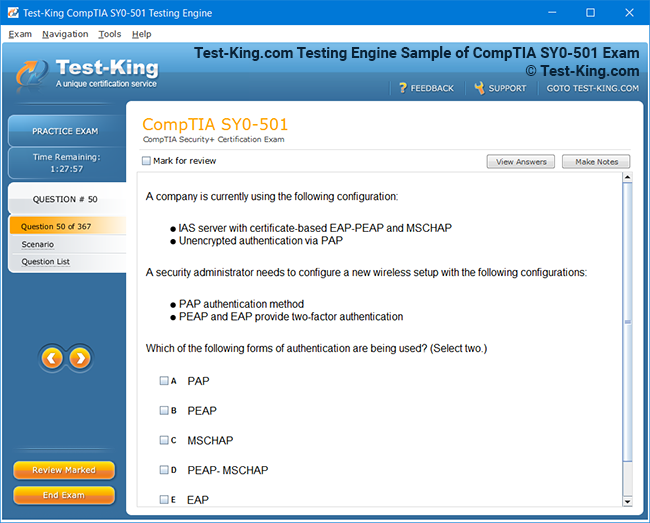
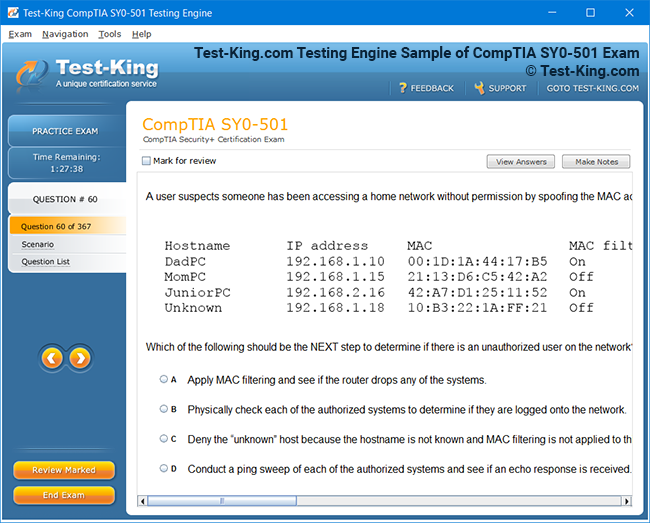
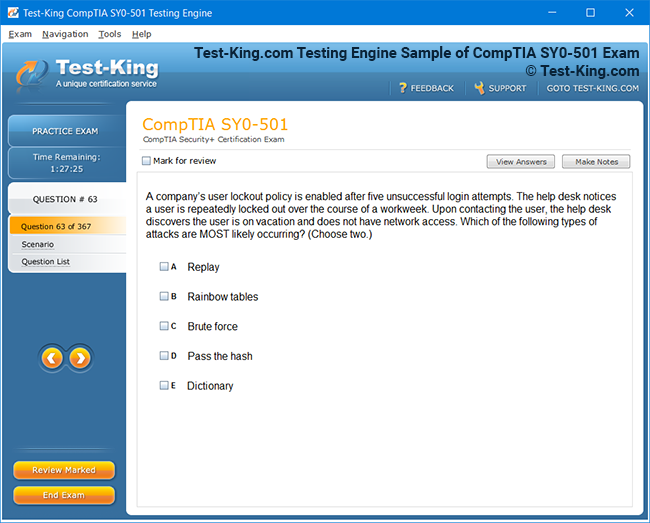
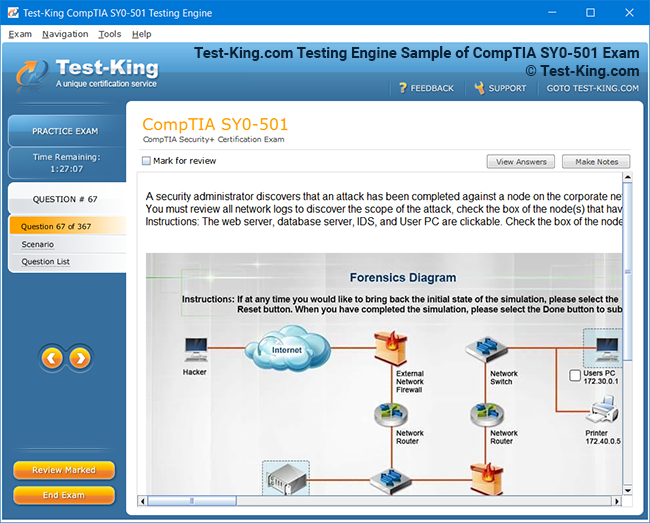
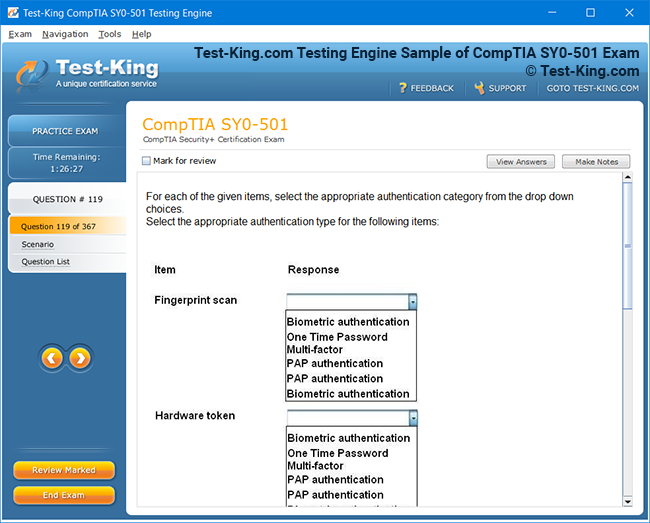
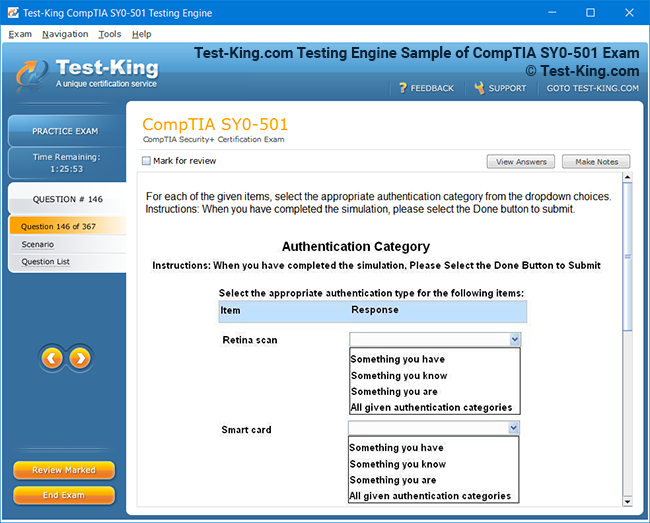
Product Screenshots
Frequently Asked Questions
How can I get the products after purchase?
All products are available for download immediately from your Member's Area. Once you have made the payment, you will be transferred to Member's Area where you can login and download the products you have purchased to your computer.
How long can I use my product? Will it be valid forever?
Test-King products have a validity of 90 days from the date of purchase. This means that any updates to the products, including but not limited to new questions, or updates and changes by our editing team, will be automatically downloaded on to computer to make sure that you get latest exam prep materials during those 90 days.
Can I renew my product if when it's expired?
Yes, when the 90 days of your product validity are over, you have the option of renewing your expired products with a 30% discount. This can be done in your Member's Area.
Please note that you will not be able to use the product after it has expired if you don't renew it.
How often are the questions updated?
We always try to provide the latest pool of questions, Updates in the questions depend on the changes in actual pool of questions by different vendors. As soon as we know about the change in the exam question pool we try our best to update the products as fast as possible.
How many computers I can download Test-King software on?
You can download the Test-King products on the maximum number of 2 (two) computers or devices. If you need to use the software on more than two machines, you can purchase this option separately. Please email support@test-king.com if you need to use more than 5 (five) computers.
What is a PDF Version?
PDF Version is a pdf document of Questions & Answers product. The document file has standart .pdf format, which can be easily read by any pdf reader application like Adobe Acrobat Reader, Foxit Reader, OpenOffice, Google Docs and many others.
Can I purchase PDF Version without the Testing Engine?
PDF Version cannot be purchased separately. It is only available as an add-on to main Question & Answer Testing Engine product.
What operating systems are supported by your Testing Engine software?
Our testing engine is supported by Windows. Andriod and IOS software is currently under development.
Top AHIMA Exams
AHIMA-Approved Continuing Education for Clinical Documentation Improvement Practitioners (CDIP)
In the contemporary healthcare landscape, professionals who possess a thorough comprehension of clinical documentation improvement hold a unique advantage. Certified Documentation Improvement Practitioners, credentialed through the American Health Information Management Association, are increasingly pivotal in navigating complex regulatory frameworks such as ARRA and HITECH. The ability to accurately capture patient health information, comply with stringent compliance standards, and facilitate seamless audits is no longer a supplementary skill; it has become an indispensable element of professional competence in health informatics.
Attaining certification demonstrates more than a foundational knowledge of clinical documentation; it signifies mastery in translating patient encounters into precise records that support clinical, financial, and operational outcomes. Those who have invested in their certification showcase to employers that they possess analytical acuity in assessing medical records, a sophisticated understanding of the intricacies of coding, and the capacity to influence documentation practices across multidisciplinary teams. Maintaining certification also reflects a commitment to continuous professional development, underscoring the practitioner's dedication to remaining at the forefront of evolving healthcare standards.
Professionals equipped with this certification often find themselves at the intersection of clinical care and administrative oversight. Their expertise is crucial in enhancing the quality of patient data, reducing discrepancies that could compromise reimbursement, and ensuring that health records faithfully represent patient conditions and interventions. The CDIP credential, therefore, is not merely an academic achievement; it is a testament to one’s role as a steward of patient information and a leader within the broader health informatics community.
Eligibility and Pathways to Certification
Earning the CDIP credential requires a combination of formal education, professional experience, and specialized examination. Individuals may qualify through a variety of avenues, reflecting the diverse professional backgrounds present in healthcare. One path requires two years of hands-on clinical documentation improvement experience in conjunction with established credentials such as RHIA, RHIT, CCS, or CCS-P, or holding an advanced professional degree such as RN, MD, or DO. These qualifications ensure that candidates have a well-rounded perspective on both the clinical and administrative facets of healthcare documentation.
Alternatively, individuals who possess an Associate’s degree supplemented with coursework in medical terminology, anatomy, and physiology may also pursue certification, provided they have accrued three years of experience in clinical documentation improvement. This pathway acknowledges the value of formal education while emphasizing the necessity of practical, experiential learning in clinical environments. Both routes culminate in a rigorous multiple-choice examination designed to assess comprehensive knowledge of documentation standards, coding accuracy, regulatory compliance, and the practical application of these skills in real-world settings.
The journey to certification does not conclude with passing the exam. Certified practitioners must engage in continuous learning, accruing 30 approved continuing education credits over each two-year period to sustain their credential. This requirement fosters a culture of perpetual growth, encouraging professionals to stay abreast of emerging technologies, evolving legislation, and best practices in clinical documentation. Such ongoing education not only preserves the value of the certification but also enhances a practitioner’s capacity to implement innovative strategies that improve patient care and operational efficiency.
Earning Continuing Education Credits Online
The contemporary professional seeking to maintain their credential often balances demanding clinical responsibilities with the need for continued education. Online learning platforms offer an optimal solution, providing flexibility without compromising quality. These programs cover complex topics such as leveraging metrics to evaluate documentation programs, navigating the challenges posed by hybrid medical records, and understanding the nuances of coding and documentation for distinct services.
Courses are meticulously crafted by recognized experts in clinical documentation and healthcare service delivery, ensuring that participants not only meet their biennial training requirements but also gain practical insights applicable to their daily work. The structure of these programs facilitates learning at a self-directed pace, enabling participants to integrate theoretical knowledge with the realities of clinical practice. Live webinars complement self-paced modules, allowing interaction with instructors and peers, fostering a community of learning where complex cases and real-world dilemmas can be discussed and resolved collaboratively.
Continuing education in this format provides more than mere compliance with certification requirements. It encourages critical thinking, analytical assessment, and the ability to apply evidence-based practices in dynamic healthcare environments. As documentation practices evolve in response to technological advancements and regulatory shifts, online learning ensures that practitioners remain proficient, adaptive, and informed. The skills acquired through such programs translate into more accurate patient records, improved audit performance, and enhanced communication among clinical and administrative teams.
Advantages of CDIP Certification in Career Advancement
Holding a CDIP credential confers tangible benefits in professional development. Beyond enhancing credibility with current and prospective employers, it positions individuals for leadership roles within clinical documentation and health information management. Organizations increasingly rely on certified practitioners to guide documentation initiatives, mentor staff, and develop strategies that optimize compliance and patient care outcomes. The credential signals a level of expertise that distinguishes candidates in competitive job markets, facilitating career mobility and the opportunity to influence organizational policies and practices.
The impact of certification extends to financial considerations as well. Certified practitioners often experience increased earning potential, reflecting the specialized skill set they bring to their organizations. Their proficiency in evaluating documentation, identifying gaps, and implementing corrective measures contributes directly to operational efficiency and financial accuracy. This dual focus on quality and compliance underscores the unique value that certified professionals provide, demonstrating how advanced knowledge of documentation standards can translate into organizational and personal growth.
Maintaining certification also aligns with broader professional aspirations. As healthcare becomes increasingly data-driven, the capacity to accurately capture, analyze, and apply patient information is paramount. CDIP-certified individuals are equipped to lead initiatives that enhance data integrity, support evidence-based decision-making, and facilitate seamless integration between clinical, administrative, and technological domains. Their expertise positions them as invaluable contributors to the ongoing evolution of health informatics and clinical documentation improvement.
Integrating Certification Knowledge into Daily Practice
The practical application of knowledge acquired through certification is essential for maximizing its benefits. Practitioners are expected to employ their understanding of documentation standards, coding principles, and compliance requirements in everyday scenarios, from reviewing patient charts to advising clinical teams. By translating theoretical knowledge into operational strategies, certified professionals ensure that health records accurately reflect patient encounters, support clinical decision-making, and comply with external regulatory expectations.
Furthermore, certified practitioners often serve as mentors and educators within their organizations, guiding colleagues in best practices and fostering a culture of continuous improvement. This leadership role enhances organizational effectiveness, as accurate and complete documentation is central to quality care delivery, reimbursement accuracy, and legal compliance. By applying certification knowledge proactively, practitioners not only enhance their personal career trajectory but also contribute to the broader advancement of health information management within their institutions.
The Role of Continuing Education in Maintaining Certification
Continuing education is not merely a procedural requirement for certified professionals; it is an essential mechanism for sustaining expertise in an ever-evolving healthcare environment. The field of clinical documentation improvement demands precision, analytical rigor, and an intimate understanding of regulatory frameworks that shape healthcare delivery. Those who pursue ongoing education demonstrate a commitment to excellence, ensuring that their skills remain attuned to contemporary standards, coding guidelines, and documentation practices.
Earning credits through structured online courses or live webinars allows professionals to expand their comprehension of nuanced clinical scenarios and the complexities of patient records. Courses designed by seasoned experts offer insights into using metrics to evaluate documentation programs effectively, identifying discrepancies that could affect reimbursement, and understanding the implications of hybrid medical record systems. By engaging in such programs, practitioners acquire not only the necessary continuing education credits but also a deeper appreciation for the interplay between accurate documentation, patient outcomes, and organizational compliance.
The requirement to complete a specified number of credits every two years fosters an ethos of perpetual learning. This process ensures that practitioners remain proficient in emerging technologies, coding updates, and legislative changes. Through consistent engagement with educational resources, professionals refine their ability to interpret and capture intricate clinical data, apply evidence-based practices, and guide organizational initiatives that enhance documentation quality. In this manner, continuing education transcends obligation, becoming a strategic tool for professional development and influence within the healthcare environment.
The Intersection of Clinical Expertise and Administrative Acumen
Certified practitioners operate at the intersection of clinical care and administrative oversight. Their role involves meticulous review of patient records, identification of documentation gaps, and collaboration with multidisciplinary teams to ensure that clinical data is comprehensive, accurate, and compliant with regulatory standards. This dual focus requires both clinical acumen and administrative dexterity, as practitioners must interpret medical information and translate it into actionable, compliant documentation.
Practical experience is essential in cultivating this dual capability. Professionals who have accumulated years of direct clinical documentation improvement experience develop a keen eye for subtle inconsistencies in patient records, an understanding of coding nuances, and the ability to anticipate areas of potential noncompliance. Certification validates this expertise, signaling to employers that the individual possesses a sophisticated understanding of the technical, regulatory, and operational aspects of healthcare documentation. Moreover, it establishes the practitioner as a trusted resource capable of guiding policy, training staff, and optimizing documentation processes.
Optimizing Workflow Through Advanced Documentation Practices
The integration of certification knowledge into daily workflows yields tangible benefits for both the practitioner and the organization. By employing structured methodologies to review and enhance documentation, professionals can improve the clarity, accuracy, and completeness of patient health records. This, in turn, supports clinical decision-making, facilitates accurate reimbursement, and ensures compliance with external audits.
Advanced documentation practices involve a careful balance of precision and efficiency. Practitioners learn to prioritize critical elements, recognize patterns in clinical data, and employ coding strategies that reflect the full scope of patient care. Education on these methodologies equips professionals with the ability to evaluate documentation programs using measurable metrics, providing leadership with data-driven insights to refine policies, allocate resources, and enhance overall operational performance. By adopting these practices, practitioners not only safeguard organizational integrity but also contribute to a culture of continuous improvement that permeates clinical and administrative domains.
Expanding Professional Influence and Leadership
Certification offers a platform for expanding influence within healthcare organizations. Professionals who have attained advanced credentials are often called upon to mentor colleagues, design training programs, and participate in cross-functional committees. Their expertise enables them to identify areas where documentation can be strengthened, propose process improvements, and guide teams in implementing best practices that align with regulatory expectations.
Leadership in this context is both technical and strategic. Practitioners leverage their knowledge to shape organizational culture, ensuring that staff at all levels understand the importance of precise clinical documentation. This influence extends beyond immediate teams, affecting organizational policies, compliance outcomes, and the quality of patient care. Through active engagement in professional development, practitioners cultivate a reputation for reliability, insight, and innovation, reinforcing the value of certification in achieving career advancement and recognition within the health informatics community.
Navigating the Challenges of Hybrid Medical Records
Healthcare organizations increasingly employ hybrid medical records, combining traditional paper-based documentation with electronic health record systems. This evolution presents both opportunities and challenges for certified practitioners, who must ensure that information is accurately captured, reconciled, and accessible across multiple platforms. Education in this area focuses on understanding the nuances of hybrid systems, identifying potential documentation discrepancies, and implementing strategies to maintain data integrity.
Practitioners trained in hybrid record management develop skills in cross-referencing entries, auditing for completeness, and ensuring that clinical information aligns with coding and billing requirements. They learn to mitigate risks associated with incomplete or inconsistent documentation and to guide teams in adopting standardized practices that support accurate reporting. By mastering these challenges, certified professionals enhance the reliability of patient data, streamline workflows, and reduce the potential for errors that could impact clinical outcomes or organizational compliance.
Enhancing Analytical Skills Through Metrics and Data Interpretation
A critical component of clinical documentation improvement involves the use of metrics to evaluate program effectiveness. Certified practitioners are trained to analyze documentation trends, identify areas of underperformance, and implement corrective strategies that elevate the quality of patient records. Education emphasizes the interpretation of quantitative and qualitative data, enabling practitioners to translate observations into actionable recommendations.
Metrics-driven evaluation fosters a culture of accountability and precision. Practitioners use benchmarks to assess documentation completeness, accuracy, and timeliness, and to identify patterns that may indicate training needs or process gaps. By integrating analytical skills with clinical expertise, certified professionals provide leadership with insights that drive strategic decisions, optimize resource allocation, and enhance overall patient care. The ability to harness data effectively underscores the unique value of certification in supporting operational excellence and regulatory compliance.
Leveraging Certification for Career Advancement
Professional recognition and career growth are natural outcomes of certification. Individuals who have attained advanced credentials are often sought for positions that demand both technical proficiency and strategic oversight. Their expertise enables them to influence policy, design training initiatives, and ensure that documentation practices meet or exceed industry standards.
Career advancement is not limited to title or salary. Certified practitioners gain opportunities to participate in organizational decision-making, shape clinical documentation strategies, and collaborate with diverse teams to implement systemic improvements. The credibility conferred by certification enhances professional mobility, opening doors to roles in larger healthcare systems, consulting organizations, and policy development entities. By consistently applying certification knowledge, practitioners establish themselves as indispensable assets whose contributions extend beyond immediate responsibilities to influence organizational success and the broader healthcare ecosystem.
Integrating Evidence-Based Practices into Documentation
Evidence-based practices are central to contemporary healthcare, and certified practitioners play a crucial role in translating clinical knowledge into accurate documentation. Education emphasizes the integration of best practices with regulatory requirements, ensuring that patient records reflect both clinical realities and compliance standards. Practitioners learn to evaluate documentation against evidence-based guidelines, identify deviations, and implement corrective measures that support quality care and operational integrity.
The incorporation of evidence-based approaches enhances the reliability of health records, facilitates clinical decision-making, and reduces the likelihood of discrepancies that could affect reimbursement or audits. Certified professionals are trained to guide clinical teams in adopting standardized practices, ensuring consistency across departments and optimizing the accuracy of patient data. This integration of evidence-based knowledge with practical documentation skills represents a hallmark of professional excellence and reinforces the value of ongoing education in sustaining certification.
The Strategic Importance of Documentation in Healthcare
Clinical documentation serves as the backbone of healthcare operations, supporting patient care, financial accuracy, and regulatory compliance. Certified practitioners recognize the strategic importance of their work, understanding that each entry in a health record has implications for patient outcomes, organizational performance, and compliance adherence. Education emphasizes the critical role of documentation in shaping organizational strategy, guiding policy decisions, and supporting operational efficiency.
By approaching documentation with a strategic mindset, practitioners enhance the overall quality of care and contribute to the development of robust health information management systems. Their expertise ensures that records are complete, accurate, and reflective of the full spectrum of patient care, enabling healthcare organizations to operate efficiently while maintaining compliance with evolving regulatory standards. This strategic perspective underscores the indispensable role of certification in fostering both professional development and organizational success.
The Importance of Specialized Knowledge in Healthcare Documentation
In the increasingly complex ecosystem of healthcare, professionals who demonstrate expertise in clinical documentation improvement occupy a critical role. The ability to ensure that patient records are precise, comprehensive, and compliant with regulatory mandates is a defining characteristic of those who pursue advanced certification. Certified practitioners not only safeguard the integrity of health information but also influence the operational efficiency and financial accuracy of healthcare organizations.
Acquiring specialized knowledge in this domain requires a sophisticated understanding of medical terminology, anatomy, physiology, and coding principles. Professionals must be adept at interpreting intricate patient data, capturing the nuances of clinical encounters, and translating these details into standardized documentation that meets both internal and external expectations. This proficiency enables organizations to navigate complex audits, ensure compliance with ARRA and HITECH standards, and optimize reimbursement processes. The value of certification lies not solely in credentialing but in the practical application of knowledge to improve patient care, enhance data quality, and streamline administrative processes.
Pathways to Achieving Certification
Certification in clinical documentation improvement is designed to validate both academic preparation and experiential expertise. Individuals with two years of direct experience in clinical documentation improvement, combined with credentials such as RHIA, RHIT, CCS, or CCS-P, or advanced professional degrees like RN, MD, or DO, are eligible to pursue certification. This pathway emphasizes the integration of practical experience with formal education, ensuring that candidates possess the clinical insight and technical competence necessary to excel.
For those with an Associate’s degree, eligibility is determined by completion of coursework in medical terminology, anatomy, and physiology, coupled with three years of professional experience in clinical documentation improvement. This alternative pathway recognizes the importance of foundational knowledge and practical application, reinforcing the principle that effective documentation relies on both education and hands-on experience. Certification is awarded following successful completion of a comprehensive multiple-choice examination that evaluates knowledge in documentation standards, coding, compliance, and the practical application of skills within diverse clinical environments.
Maintaining certification requires continuous professional development, with practitioners completing 30 approved continuing education credits every two years. This ensures that certified individuals remain current with emerging healthcare regulations, technological innovations, and best practices in clinical documentation, reinforcing the ongoing relevance and value of their expertise.
Leveraging Online Education for Continued Expertise
Online learning platforms have transformed the way certified professionals maintain and expand their competencies. The flexibility of virtual education allows practitioners to integrate training into demanding schedules without compromising the quality of learning. Courses in clinical documentation improvement cover critical topics such as program evaluation through metrics, managing hybrid medical records, and navigating the complexities of documentation and coding for distinct services.
These programs, developed by seasoned experts, provide not only the required continuing education credits but also practical strategies that can be applied directly to professional responsibilities. The curriculum emphasizes real-world challenges, offering guidance on improving documentation quality, ensuring compliance, and optimizing clinical workflows. Practitioners gain insights into the systematic evaluation of health records, methods for detecting documentation gaps, and techniques for implementing corrective measures that align with organizational goals.
Live webinars complement self-paced modules, allowing participants to engage in interactive discussions, analyze case studies, and share experiences with peers. This collaborative environment enhances learning by encouraging problem-solving, critical thinking, and the application of theoretical knowledge to practical scenarios. Online education thus becomes a dual-purpose tool: maintaining certification while enriching professional capability and confidence.
Applying Certification Knowledge to Daily Practice
The practical application of certification knowledge is crucial for demonstrating its value within healthcare organizations. Certified practitioners are expected to use their understanding of documentation standards and coding principles to ensure that patient records accurately reflect the clinical encounter. This includes reviewing charts for completeness, resolving inconsistencies, and advising clinical teams on best practices.
Beyond technical application, certified professionals often assume mentorship roles, guiding colleagues in improving documentation quality and compliance adherence. By fostering a culture of continuous improvement, they help ensure that healthcare organizations consistently meet internal quality benchmarks and external regulatory requirements. Their expertise facilitates better communication across departments, improves the accuracy of billing and reimbursement, and strengthens the integrity of organizational health information management systems.
Navigating the Challenges of Hybrid and Electronic Records
Healthcare organizations increasingly rely on hybrid documentation systems that combine electronic health records with traditional paper records. This evolution presents unique challenges in ensuring that data is accurately captured, reconciled, and consistently maintained across formats. Certified practitioners play a central role in addressing these challenges by implementing protocols that preserve data integrity and enhance accessibility.
Through education and experience, practitioners develop strategies to reconcile discrepancies between electronic and paper records, audit for completeness, and standardize documentation practices. Their skills ensure that patient information remains coherent and actionable, supporting clinical decision-making, facilitating reimbursement processes, and minimizing the risk of compliance violations. Mastery of hybrid systems is a distinguishing feature of certified professionals, underscoring their capacity to adapt to technological advancements while maintaining high standards of documentation accuracy.
Using Metrics to Improve Documentation Programs
Metrics are indispensable tools for assessing the effectiveness of clinical documentation programs. Certified practitioners employ quantitative and qualitative analyses to evaluate documentation completeness, accuracy, and compliance. By systematically measuring performance, they can identify trends, detect deficiencies, and implement targeted interventions that improve the quality of patient records.
The analytical skills developed through certification allow practitioners to interpret complex data and translate findings into actionable improvements. For example, audits may reveal areas where additional staff training is required, or where workflow adjustments could enhance efficiency. By integrating metrics-driven evaluation into routine practice, certified professionals contribute to a culture of accountability and continuous refinement, strengthening organizational performance and regulatory compliance.
Career Advancement Through Certification
Certification significantly influences career trajectory by distinguishing individuals as experts in clinical documentation improvement. Certified practitioners are frequently sought for roles that require both technical proficiency and strategic insight, including leadership positions, policy development, and training responsibilities. The credential signals mastery of documentation standards, coding principles, and regulatory compliance, positioning individuals to influence organizational practices and outcomes.
The career benefits of certification extend beyond immediate responsibilities. Certified practitioners gain credibility within their organizations, enhancing opportunities for promotion, professional recognition, and engagement in strategic initiatives. Their expertise allows them to participate in committees, lead documentation projects, and mentor other staff, reinforcing their influence on both clinical and administrative domains. As the healthcare landscape continues to evolve, certification ensures that professionals remain adaptable, knowledgeable, and highly valued contributors.
Integrating Evidence-Based Practice into Documentation
Evidence-based practice is foundational to contemporary healthcare, and certified practitioners are uniquely positioned to ensure that documentation reflects current standards and research. This involves evaluating clinical encounters against established guidelines, verifying the accuracy of patient data, and implementing strategies to address inconsistencies or omissions. By integrating evidence-based approaches into documentation, practitioners enhance the reliability of patient records, support clinical decision-making, and promote best practices across the organization.
Certified professionals often educate colleagues on the application of evidence-based practices in documentation, fostering consistency and quality in patient records. Their role ensures that health information not only meets regulatory requirements but also accurately represents patient care, improving the effectiveness of interventions, optimizing reimbursement, and contributing to a culture of clinical excellence.
Strategic Implications of Documentation Expertise
Documentation expertise extends beyond administrative compliance to influence the strategic direction of healthcare organizations. Certified practitioners understand that precise, complete, and accurate records are essential for operational efficiency, financial stability, and quality patient care. Their work informs decision-making processes, supports policy development, and facilitates data-driven organizational strategies.
By approaching documentation with a strategic perspective, practitioners enhance the organization’s ability to respond to audits, implement quality improvement initiatives, and leverage data for clinical research. Their contributions are instrumental in maintaining the integrity of health information systems and ensuring that patient care, financial operations, and regulatory compliance remain aligned. This strategic understanding is a hallmark of professional excellence, reflecting the broader impact of certification on healthcare operations.
Leadership and Mentorship in Clinical Documentation
Certified practitioners often assume leadership roles, guiding teams in adopting best practices, mentoring colleagues, and implementing organizational initiatives that enhance documentation quality. Their influence extends to shaping institutional policies, developing training programs, and fostering a culture of continuous improvement. Leadership in this domain requires a combination of technical expertise, strategic insight, and interpersonal skill, enabling practitioners to drive meaningful change across clinical and administrative functions.
Through mentorship, certified professionals cultivate knowledge and skills in others, ensuring that best practices are consistently applied and that the organization maintains a high standard of documentation quality. Their leadership strengthens operational effectiveness, enhances compliance, and contributes to a cohesive, informed, and capable workforce.
Advancing Skills Through Specialized Training
In modern healthcare systems, professionals who excel in clinical documentation improvement occupy a crucial position. The precision of patient records, the fidelity of coded information, and compliance with evolving regulations hinge on the expertise of certified practitioners. Continuous education serves as a cornerstone for maintaining proficiency, providing practitioners with exposure to emerging standards, sophisticated methodologies, and novel strategies that optimize documentation quality.
Training programs designed for advanced practitioners encompass a broad spectrum of topics, including metrics for evaluating program effectiveness, strategies to manage hybrid and electronic medical records, and techniques for accurate coding in complex clinical scenarios. Through structured courses, individuals not only fulfill certification maintenance requirements but also develop practical skills that enhance operational efficiency and support better patient outcomes. The cumulative knowledge gained through these educational experiences equips practitioners to navigate multifaceted challenges, ensuring that documentation remains a reliable foundation for both clinical and administrative processes.
Applying Certification Expertise in Organizational Settings
The impact of certification is most evident in the daily responsibilities of healthcare professionals. Certified practitioners are tasked with reviewing and refining patient records, identifying inconsistencies, and collaborating with clinical teams to improve the clarity and accuracy of documentation. This role requires a combination of analytical reasoning, clinical knowledge, and administrative foresight.
Individuals who integrate their certification expertise into organizational practices influence workflow design, standard operating procedures, and compliance strategies. They often lead quality improvement initiatives, providing guidance on best practices for record-keeping, coding accuracy, and regulatory adherence. Their interventions ensure that documentation processes are streamlined, errors are minimized, and the organization can respond effectively to audits or regulatory inquiries. The capacity to translate theoretical knowledge into operational improvements underscores the tangible benefits of certification within healthcare institutions.
Enhancing Documentation in Hybrid and Electronic Records
The proliferation of hybrid medical records, which combine traditional paper documentation with electronic health record systems, presents both opportunities and challenges. Certified practitioners play a critical role in ensuring that data is consistently accurate, complete, and accessible across all platforms. Their training emphasizes the reconciliation of discrepancies, standardization of entries, and implementation of protocols that maintain the integrity of patient information.
Proficiency in hybrid record management enables practitioners to identify potential areas of risk, mitigate errors, and provide guidance to clinical teams on maintaining comprehensive and compliant documentation. Their oversight ensures that patient data is actionable, reliable, and fully representative of clinical encounters. This capability not only safeguards the organization against compliance issues but also enhances the quality of patient care by providing clinicians with accurate and timely information.
Leveraging Metrics to Strengthen Documentation Programs
The systematic use of metrics is indispensable for evaluating the effectiveness of clinical documentation initiatives. Certified practitioners apply quantitative and qualitative measures to assess completeness, accuracy, and timeliness in patient records. These analyses identify areas for improvement, reveal patterns that may indicate training needs, and provide evidence for targeted interventions.
Metrics-driven evaluation enables organizations to make data-informed decisions, optimize resource allocation, and enhance compliance with regulatory requirements. Practitioners skilled in interpreting performance data can translate findings into actionable strategies, improving documentation practices and reinforcing accountability at all organizational levels. This analytical approach ensures that documentation programs are not only maintained but continuously refined to meet evolving standards and organizational objectives.
Career Growth Through Advanced Certification
Certification in clinical documentation improvement significantly enhances professional trajectories. Individuals who possess this credential are often considered for roles requiring both clinical insight and strategic oversight. Their expertise in coding, documentation standards, and regulatory compliance positions them to influence policy development, lead training programs, and manage documentation initiatives that affect organizational performance.
The benefits of certification extend beyond immediate technical skills. Certified professionals gain recognition as thought leaders within their organizations, contributing to strategic discussions and quality improvement projects. Their expertise supports career advancement, providing access to higher-level positions, leadership opportunities, and engagement in projects that shape institutional practices. By continuously applying their certification knowledge, practitioners strengthen their professional profile while contributing to the advancement of the broader healthcare system.
Integrating Evidence-Based Practices into Documentation
Evidence-based practices are essential for ensuring that clinical documentation accurately reflects patient care and supports optimal outcomes. Certified practitioners are trained to evaluate records against established guidelines, identify inconsistencies, and implement corrective strategies that align with both clinical best practices and regulatory requirements.
Incorporating evidence-based approaches into documentation enhances the reliability and credibility of patient records. It also improves the efficiency of clinical decision-making, reduces the likelihood of errors, and ensures that healthcare organizations can demonstrate compliance with auditing and reporting standards. Practitioners often play an educational role, guiding colleagues in adopting consistent practices that reflect the latest evidence, reinforcing the quality and integrity of the documentation process.
Strategic Importance of Clinical Documentation
Clinical documentation serves as the backbone of healthcare operations, influencing patient care, financial accuracy, and regulatory adherence. Certified practitioners understand that the quality of documentation has direct implications for organizational effectiveness. Accurate, comprehensive records support decision-making, facilitate audits, and contribute to the institution’s strategic objectives.
By applying a strategic lens to documentation, practitioners ensure that health information is actionable and reliable. Their work informs policy development, quality improvement initiatives, and operational planning. The ability to align documentation practices with organizational goals demonstrates the multifaceted value of certification, reinforcing its importance beyond individual professional development to include systemic impact within healthcare organizations.
Mentorship and Leadership in Clinical Documentation
Leadership is a natural extension of certification, as experienced practitioners are frequently called upon to mentor colleagues, lead documentation initiatives, and influence organizational practices. Their guidance ensures that best practices are consistently applied, staff are trained in proper techniques, and documentation processes meet high standards of accuracy and compliance.
Through mentorship, certified professionals cultivate a culture of continuous improvement and knowledge sharing. They facilitate the transfer of expertise, ensuring that clinical and administrative teams are equipped to maintain high-quality records. Leadership in this context encompasses technical proficiency, strategic insight, and interpersonal skill, allowing practitioners to drive meaningful improvements and reinforce the value of clinical documentation across all levels of the organization.
Navigating Regulatory Complexity
Healthcare regulations are continually evolving, and certified practitioners must remain adept at interpreting and applying these requirements to maintain compliance. Knowledge of ARRA, HITECH, and other regulatory frameworks allows practitioners to guide organizations in implementing documentation practices that meet legal standards while supporting operational efficiency.
Practitioners trained in regulatory compliance can identify potential vulnerabilities in documentation, advise on corrective actions, and ensure that policies are updated to reflect current requirements. Their expertise minimizes risk, supports audit readiness, and ensures that patient records provide an accurate and defensible account of care. By integrating regulatory knowledge with clinical and administrative proficiency, certified professionals enhance both organizational resilience and patient safety.
Optimizing Workflow and Operational Efficiency
The role of certified practitioners extends to improving organizational workflows and operational efficiency. By analyzing documentation processes, identifying bottlenecks, and implementing standardized protocols, practitioners enhance the timeliness, accuracy, and usability of patient records. Their interventions streamline communication between departments, reduce errors, and support efficient billing and reimbursement procedures.
Optimization of workflow requires both analytical skills and practical knowledge of clinical operations. Certified professionals leverage their training to design interventions that balance compliance with operational demands, ensuring that documentation processes contribute positively to overall organizational performance. Their contributions demonstrate the practical value of certification in creating systems that are both effective and sustainable.
Elevating Professional Expertise Through Certification
In the evolving landscape of healthcare, professionals who achieve certification in clinical documentation improvement occupy a position of strategic importance. The ability to ensure that patient records are precise, complete, and aligned with regulatory standards has become a defining feature of effective health information management. Certified practitioners are not only responsible for safeguarding data integrity but also for optimizing clinical workflows, supporting reimbursement accuracy, and facilitating compliance with audits and legislative mandates.
Certification represents an acknowledgment of both experience and academic preparation. Individuals who hold this credential demonstrate mastery in interpreting complex clinical information, translating encounters into accurate documentation, and guiding organizational practices to meet contemporary standards. The ongoing commitment to education required to maintain certification reinforces expertise, ensuring that practitioners remain conversant with technological innovations, evolving regulatory requirements, and best practices in clinical documentation.
Integrating Knowledge Into Daily Practice
Certified practitioners apply their knowledge consistently to improve organizational outcomes. Reviewing patient charts, identifying gaps, and advising clinical teams on accurate documentation are daily responsibilities that demand analytical precision and clinical insight. By integrating certification knowledge into routine practice, professionals enhance the reliability of health records, support decision-making, and foster efficiency in administrative and clinical workflows.
In addition to technical application, practitioners often serve as mentors within their organizations. Their guidance ensures that colleagues adopt standardized procedures, understand coding nuances, and comply with regulatory expectations. By cultivating a culture of continuous improvement, certified professionals reinforce the quality and consistency of documentation, thereby enhancing the overall effectiveness of healthcare operations.
Managing Hybrid and Electronic Health Records
The integration of hybrid and electronic health record systems introduces complexity into clinical documentation. Certified practitioners are equipped to navigate these challenges, ensuring that information is consistent, reconciled, and accessible across multiple formats. Their expertise allows for the identification of discrepancies, the implementation of standardized procedures, and the maintenance of data integrity throughout the documentation lifecycle.
Proficiency in hybrid systems ensures that patient information remains accurate and actionable, supporting clinical decision-making, reimbursement, and regulatory compliance. Practitioners trained in these systems are adept at auditing records, resolving inconsistencies, and training staff in proper documentation techniques. Their role is critical in maintaining the fidelity of health information while leveraging technological advancements to improve operational efficiency.
Utilizing Metrics for Continuous Improvement
The application of metrics is essential for evaluating the effectiveness of clinical documentation programs. Certified practitioners employ both quantitative and qualitative measures to assess accuracy, completeness, and timeliness in patient records. These evaluations reveal patterns of deficiency, highlight opportunities for process optimization, and provide a foundation for targeted interventions.
Metrics-driven analysis empowers organizations to implement evidence-based improvements, allocate resources effectively, and maintain accountability at every level. By interpreting and acting upon data, practitioners can refine documentation practices, reduce errors, and enhance compliance. This analytical approach transforms documentation from a routine task into a strategic tool for operational excellence, reflecting the broader impact of certification on organizational performance.
Career Development and Leadership Opportunities
Certification opens avenues for professional growth, positioning individuals for roles that require both clinical expertise and strategic vision. Certified practitioners frequently assume leadership responsibilities, guiding documentation initiatives, developing training programs, and influencing policy decisions within their organizations. Their skills in coding, compliance, and program evaluation distinguish them as valuable contributors to both operational and strategic objectives.
Leadership extends beyond formal titles; it encompasses mentoring, policy guidance, and the ability to shape organizational culture. Certified professionals provide direction in implementing best practices, addressing documentation gaps, and fostering continuous improvement. This leadership not only advances career prospects but also ensures that organizations maintain high standards of accuracy, efficiency, and regulatory adherence.
Evidence-Based Practices in Documentation
Evidence-based practice is central to the role of certified practitioners, ensuring that documentation accurately reflects patient care and supports optimal outcomes. Professionals are trained to evaluate clinical records against established guidelines, identify inconsistencies, and implement corrective actions. By integrating evidence-based approaches, practitioners enhance the reliability and credibility of documentation, support informed clinical decision-making, and facilitate accurate reimbursement and compliance.
Certified individuals often disseminate knowledge throughout their organizations, educating colleagues on the application of evidence-based practices. This promotes uniformity, enhances quality, and reinforces the standardization of documentation procedures. The integration of research, clinical insight, and regulatory understanding epitomizes the professional competence of those who maintain certification.
Strategic Value of Documentation Expertise
Clinical documentation serves as a critical foundation for healthcare operations, influencing patient care, financial accuracy, and regulatory compliance. Certified practitioners recognize that accurate records are integral to strategic planning, quality initiatives, and operational management. By ensuring that documentation meets rigorous standards, professionals support organizational decision-making, guide resource allocation, and improve the overall efficiency of healthcare delivery.
Approaching documentation strategically allows practitioners to anticipate potential challenges, streamline processes, and implement practices that optimize both clinical and administrative outcomes. Their expertise contributes to the development of resilient systems capable of adapting to evolving standards, technological innovations, and legislative requirements, thereby reinforcing the indispensable role of certification within healthcare organizations.
Mentorship and Professional Influence
Certified practitioners often extend their influence through mentorship, guiding teams in the adoption of best practices, offering training, and advising on the interpretation of complex documentation requirements. Their leadership fosters a culture of accountability, consistency, and continuous improvement across departments.
Through mentorship, professionals ensure that knowledge is transferred effectively, colleagues develop competence in documentation standards, and organizations achieve higher levels of compliance and operational efficiency. The combination of technical expertise, strategic insight, and interpersonal skill positions certified practitioners as catalysts for organizational improvement and professional development.
Navigating Regulatory and Compliance Challenges
Regulatory complexity is a defining characteristic of contemporary healthcare, and certified practitioners must remain adept at interpreting and applying relevant legislation. Knowledge of ARRA, HITECH, and other regulatory frameworks allows professionals to guide organizations in developing documentation practices that meet compliance requirements while supporting operational goals.
Practitioners are skilled at identifying vulnerabilities, advising corrective measures, and ensuring that records accurately reflect clinical encounters. Their expertise in regulatory adherence minimizes risk, supports audit preparedness, and reinforces the reliability of patient information. By combining regulatory knowledge with clinical insight and administrative competence, certified individuals provide organizations with robust solutions that safeguard both operational integrity and patient safety.
Optimizing Operational Efficiency Through Documentation
The impact of certified practitioners extends to operational efficiency, as they analyze workflows, identify inefficiencies, and implement protocols that enhance documentation quality. Streamlined processes reduce redundancy, prevent errors, and facilitate effective communication across clinical and administrative teams.
Optimization of documentation workflows requires analytical judgment, clinical understanding, and practical application of certification knowledge. Practitioners develop strategies that ensure compliance, maintain accuracy, and support timely decision-making. Their interventions strengthen organizational performance, demonstrating the practical significance of advanced certification in improving both healthcare delivery and administrative operations.
Conclusion
The body of work on clinical documentation improvement illustrates the multifaceted significance of certification in contemporary healthcare. Certified practitioners serve as the linchpins of accurate, comprehensive, and compliant patient records, ensuring that documentation aligns with clinical realities, coding standards, and regulatory mandates. Their expertise bridges the gap between clinical care and administrative oversight, providing organizations with reliable health information that supports decision-making, operational efficiency, and financial accuracy.
Achieving and maintaining certification reflects a combination of rigorous education, practical experience, and ongoing professional development. Practitioners who pursue continuing education demonstrate a commitment to excellence, remaining conversant with evolving legislation, technological advancements, and emerging best practices. This dedication enhances their ability to evaluate documentation programs using metrics, manage hybrid and electronic records, and integrate evidence-based practices into daily workflows.
The impact of certified professionals extends beyond technical competence. They often assume leadership roles, mentor colleagues, influence organizational policy, and cultivate a culture of continuous improvement. Their strategic application of knowledge improves patient care quality, supports compliance with audits and regulations, and strengthens the integrity of health information management systems.
By combining analytical acuity, clinical insight, and administrative proficiency, certified practitioners elevate the standard of documentation within healthcare institutions. Their contributions ensure that records are precise, actionable, and reflective of patient encounters, which in turn optimizes operational processes, enhances reimbursement accuracy, and supports informed decision-making. The holistic expertise gained through certification positions professionals as invaluable assets capable of advancing organizational goals, fostering professional growth, and sustaining high-quality patient care in a dynamic healthcare landscape.
In essence, certification in clinical documentation improvement is more than a credential; it embodies a dedication to professional excellence, strategic influence, and the continuous enhancement of healthcare delivery. Practitioners equipped with this expertise not only maintain the integrity of patient records but also play a pivotal role in shaping efficient, compliant, and resilient healthcare systems.