Certification: CHP
Certification Full Name: Certified HIPAA Professional
Certification Provider: HIPAA
Exam Code: HIO-201
Exam Name: Certified HIPAA Professional (CHP)
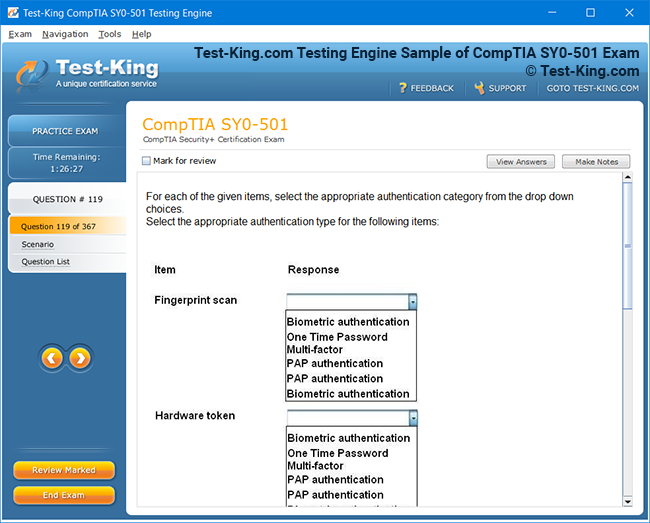
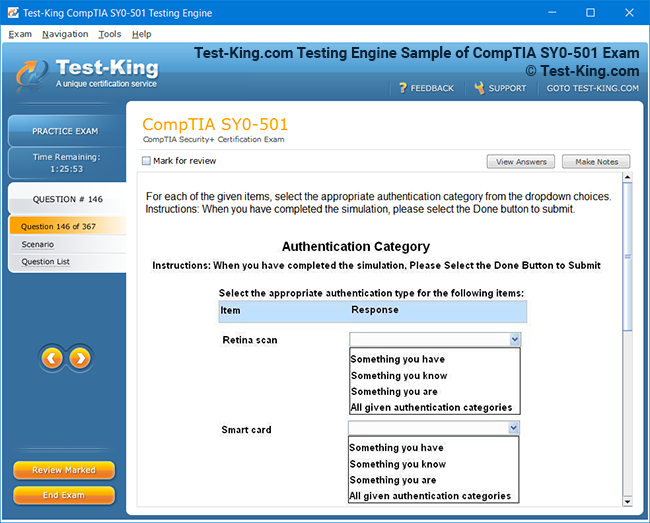
Product Screenshots
Introduction to CHP Certification and Its Importance
Healthcare has evolved into an intricate network of technology, privacy frameworks, and ethical considerations. At the heart of this transformation lies the growing necessity to protect patient information while maintaining operational efficiency. The Certified HIPAA Professional (CHP) certification embodies this mission, designed to equip healthcare professionals with the expertise required to uphold confidentiality, integrity, and compliance in an increasingly digitized healthcare landscape.
The significance of this certification stems from the Health Insurance Portability and Accountability Act (HIPAA), a cornerstone regulation that governs the protection and management of patient health data across the United States. As healthcare systems expand their reliance on digital platforms, the need for qualified experts who can interpret, implement, and maintain compliance with HIPAA’s stringent mandates becomes paramount. The CHP credential validates a professional’s ability to navigate these complexities with precision, ensuring both patients’ trust and organizational accountability remain intact.
Understanding the Essence of the CHP Certification
The Certified HIPAA Professional certification represents a profound understanding of the administrative, technical, and physical safeguards essential for compliance. It is not merely a credential; it is a demonstration of mastery in one of the most critical aspects of healthcare administration—protecting sensitive health data from breaches, misuse, and negligence. Professionals who obtain this certification possess the insight to interpret regulatory language, assess risks, implement security measures, and develop privacy frameworks tailored to their organizations’ unique environments.
The genesis of the CHP credential lies in the demand for professionals capable of bridging the gap between regulation and practice. Healthcare entities—ranging from hospitals and insurance providers to research institutions and third-party service vendors—must adhere to HIPAA’s Privacy, Security, and Breach Notification Rules. A Certified HIPAA Professional ensures that these entities do not simply meet compliance for regulatory audits but cultivate a culture of ethical stewardship toward patient information. This dynamic role involves not only technical comprehension but also moral discernment and strategic foresight.
The Growing Importance of HIPAA Compliance in Modern Healthcare
The digitalization of medical records has revolutionized the healthcare sector, allowing for more efficient patient management and data sharing. However, it has also expanded the avenues for potential security breaches. The consequences of non-compliance—ranging from financial penalties to reputational damage—can be catastrophic for healthcare organizations. Hence, there is an escalating demand for individuals who understand the subtleties of HIPAA regulations and can ensure adherence across all operational layers.
HIPAA compliance is more than a legal requirement; it is a moral obligation embedded in the core values of healthcare. Patients entrust medical professionals with intimate details of their lives, expecting confidentiality as a given. When that trust is compromised, it erodes the foundation of the healthcare system itself. Certified HIPAA Professionals play a vital role in preserving this trust by ensuring that every process involving patient data—whether electronic or physical—is handled with the utmost care and compliance.
Moreover, HIPAA compliance intersects with emerging global data protection frameworks such as the General Data Protection Regulation (GDPR). For multinational healthcare organizations, this overlap underscores the necessity of professionals who understand data privacy not just from a local regulatory perspective but through an international lens. CHP-certified individuals thus hold an advantage in understanding and harmonizing compliance efforts across jurisdictions, reinforcing their indispensability in the healthcare ecosystem.
The Professional Advantage of the CHP Credential
Earning the CHP certification conveys a professional’s commitment to maintaining the highest standards of patient privacy and data protection. It symbolizes both competence and ethical integrity—qualities that healthcare organizations seek in individuals responsible for compliance oversight. Employers recognize the certification as evidence of expertise in interpreting regulatory frameworks, implementing policy, and managing risk.
Professionals who achieve the CHP credential often find themselves positioned for advancement into senior compliance, privacy, and security roles. They are trusted advisors in shaping institutional protocols, designing staff training programs, and ensuring that every department aligns with HIPAA’s expectations. Their value extends beyond compliance departments; they are integral to IT governance, data security, patient relations, and executive leadership discussions.
For individuals entering the healthcare sector, the CHP certification provides a gateway to a rewarding and stable career. It enables professionals to stand apart in a competitive job market by showcasing specialized knowledge that remains in high demand. As healthcare organizations grapple with evolving regulations and technological innovations such as telemedicine, cloud data storage, and AI-driven diagnostics, the need for certified experts who can manage privacy risks continues to surge.
The Organizational Significance of CHP Professionals
Organizations that employ CHP-certified professionals benefit from more than regulatory assurance. They cultivate resilience against potential data breaches and public scrutiny. The presence of certified staff ensures that compliance is integrated into every operational tier, from administrative procedures to clinical practices and IT infrastructures. These professionals act as internal consultants who can preemptively identify vulnerabilities, recommend preventive measures, and guide the organization toward continuous compliance readiness.
A healthcare institution with a robust HIPAA compliance culture not only avoids penalties but also gains a competitive edge. Patients, insurers, and regulatory bodies perceive such organizations as trustworthy and credible. In the current environment where cybersecurity threats evolve rapidly, maintaining a reputation for reliability and confidentiality can be as valuable as clinical excellence. The CHP-certified workforce becomes the cornerstone of this reputation, ensuring that compliance transcends checklists and evolves into an organizational ethos.
Furthermore, CHP professionals contribute to strategic decision-making processes. Their insights influence investments in secure technologies, guide policy formulation, and enhance communication between departments that traditionally operate in silos. They ensure that technological innovations are balanced with privacy imperatives, enabling progress without compromising patient trust. In essence, the certification empowers professionals to act as both guardians and innovators within their organizations.
The Evolving Landscape of Data Protection in Healthcare
As healthcare transitions into a fully digital paradigm, the parameters of HIPAA compliance continue to expand. The rise of telehealth, wearable health devices, and mobile applications has introduced new dimensions of data vulnerability. Patient information now traverses multiple platforms and networks, some of which fall outside traditional healthcare boundaries. The role of Certified HIPAA Professionals becomes increasingly pivotal in addressing these emerging complexities.
They are tasked with understanding not only traditional healthcare data systems but also the implications of modern technologies such as cloud computing, Internet of Things (IoT) devices, and artificial intelligence in healthcare analytics. Each of these innovations, while beneficial, introduces new risks to privacy and security. A Certified HIPAA Professional must be adept at identifying these risks and crafting strategies that uphold compliance without hindering technological progress.
In this ever-shifting landscape, continuous education is indispensable. HIPAA regulations themselves may not change frequently, but their interpretations and applications evolve with technological advancements and judicial precedents. CHP-certified professionals are expected to remain vigilant, proactive, and informed, ensuring that their organizations stay ahead of compliance challenges rather than reacting to them retroactively.
The Future of HIPAA Compliance and the Enduring Value of CHP Certification
The healthcare sector’s trajectory points toward an environment where data is both a critical asset and a potential liability. The future will demand an even greater synthesis of technology, ethics, and governance. In such an era, the Certified HIPAA Professional certification stands as a symbol of preparedness and accountability.
Emerging trends such as artificial intelligence-driven diagnostics, genetic data analysis, and cross-border data sharing will redefine the contours of patient privacy. As healthcare systems integrate predictive analytics and machine learning models, ensuring ethical and compliant data usage will require professionals with deep regulatory acumen and moral foresight. CHP-certified individuals will be instrumental in shaping policies that balance innovation with integrity.
The certification also positions professionals at the forefront of institutional resilience. Cybersecurity incidents, ransomware attacks, and data leaks are no longer isolated events—they have become systemic threats. A Certified HIPAA Professional’s expertise enables healthcare institutions to anticipate and mitigate these threats effectively. Their influence extends beyond policy into the organizational psyche, fostering a culture where every employee understands the sanctity of patient information.
In essence, the CHP certification is not merely an academic achievement but a professional covenant—a commitment to uphold the ethical, legal, and operational dimensions of healthcare privacy. It prepares individuals to navigate the intricacies of compliance with confidence, foresight, and empathy. As the healthcare landscape becomes more interconnected and technology-driven, the relevance of CHP-certified professionals will only continue to grow, serving as the vanguard of trust and integrity in the protection of patient data.
Eligibility and Prerequisites for CHP Certification
In the intricate ecosystem of healthcare, where data protection and compliance underpin the entire structure, the Certified HIPAA Professional certification stands as a prestigious validation of expertise and integrity. It is designed to empower healthcare professionals with the knowledge to interpret, implement, and maintain adherence to the intricate stipulations of the Health Insurance Portability and Accountability Act. However, before embarking on the journey to achieve this credential, understanding the eligibility criteria and prerequisites becomes indispensable. These requirements shape the foundation upon which the certification’s value rests, ensuring that those who pursue it possess the intellectual rigor, professional maturity, and ethical sensibility necessary for managing patient privacy and regulatory compliance.
The CHP certification does not merely signify an academic qualification; it is a professional affirmation of an individual’s competence in healthcare privacy and information security. It appeals to a wide range of professionals—from clinical administrators and compliance officers to information security analysts and policy strategists—each seeking to refine their grasp of privacy governance and safeguard patient data against evolving threats. To thrive in this domain, candidates must demonstrate a combination of educational grounding, professional experience, and intrinsic attributes that reflect diligence, analytical acuity, and ethical discernment.
Educational Background and Academic Foundation
Although there is no rigid educational barrier preventing one from pursuing the Certified HIPAA Professional credential, candidates are typically expected to possess a foundational understanding of healthcare operations, data management, or information security. Individuals who have completed formal education in healthcare administration, nursing, medical informatics, cybersecurity, business administration, or law often find themselves well-equipped for the certification process.
An undergraduate degree in any of these domains provides the conceptual grounding necessary to comprehend the complexities of healthcare compliance. Those with degrees in technology-oriented disciplines such as computer science or information systems also hold a distinct advantage, as the certification delves deeply into technical safeguards and data protection mechanisms. Similarly, professionals with academic exposure to public health or health information management understand the ethical and procedural elements that underpin patient care and privacy protection.
For individuals without formal education in healthcare or technology, the pathway remains open through professional experience and self-guided learning. Many professionals enter the field from administrative or managerial backgrounds, cultivating their understanding of HIPAA regulations through practical exposure. The certification serves as both a recognition of existing knowledge and a structured framework to enhance it further. Thus, academic credentials, while advantageous, are not the sole determinants of eligibility.
Professional Experience and Practical Exposure
Work experience plays a pivotal role in preparing candidates for the Certified HIPAA Professional certification. Those who have engaged in healthcare operations, compliance management, or IT security acquire firsthand insights into the challenges of balancing efficiency with confidentiality. Experience in roles such as compliance coordinator, health information manager, medical billing specialist, IT administrator, or patient privacy officer strengthens one’s grasp of HIPAA’s multifaceted dimensions.
Professionals who have worked within hospitals, insurance companies, healthcare consulting firms, or government health agencies often develop an innate understanding of privacy policies, risk assessments, and patient information workflows. Such exposure proves invaluable when navigating the nuances of HIPAA’s Privacy, Security, and Enforcement Rules. Even individuals from non-healthcare sectors—such as legal consulting or enterprise risk management—bring transferable skills relevant to compliance oversight, data governance, and policy enforcement.
The certification acknowledges that practical experience cultivates more than procedural understanding; it instills a sense of ethical accountability. Those accustomed to handling confidential data recognize the gravity of safeguarding patient information, not merely for regulatory compliance but as a matter of moral obligation. This experiential depth enables CHP candidates to approach the certification curriculum with contextual clarity and pragmatic insight, enriching their learning experience.
Core Skills Essential for Certification Success
Beyond academic credentials and professional tenure, certain intrinsic and developed skills define a candidate’s readiness for the CHP certification. The ability to interpret regulatory text, assess risks, and design mitigation strategies requires a blend of analytical reasoning, problem-solving, and critical thinking. A candidate must be adept at synthesizing legal frameworks with technological processes—a skill that demands both intellectual flexibility and methodical precision.
Attention to detail is paramount. HIPAA compliance depends on precise documentation, procedural accuracy, and consistent monitoring. Candidates must cultivate a meticulous approach to analyzing workflows, identifying vulnerabilities, and ensuring every safeguard aligns with the regulatory mandate.
Equally vital is communication prowess. A Certified HIPAA Professional often functions as an intermediary between technical teams, healthcare staff, and executive leadership. This necessitates the ability to articulate complex privacy concepts in accessible terms, ensuring that all stakeholders comprehend their responsibilities in maintaining compliance. A strong command of both written and verbal communication enables candidates to draft policies, conduct training sessions, and prepare reports with clarity and authority.
Ethical judgment forms the moral nucleus of this certification. Candidates must embody integrity, discretion, and responsibility, as their decisions often influence the handling of sensitive patient data. An ethical lapse, even unintentional, can compromise institutional trust and patient safety. Therefore, the certification process demands individuals who not only understand the letter of the law but uphold its spirit through conscientious practice.
The Role of Foundational Knowledge in Medical Ethics and Information Privacy
A profound understanding of medical ethics and information privacy is indispensable for any professional aspiring to attain the CHP certification. Healthcare, at its core, revolves around trust—the implicit agreement that patient information will remain confidential and used solely for the purpose of care. This principle, deeply embedded in medical ethics, aligns seamlessly with the objectives of HIPAA. Candidates familiar with ethical doctrines such as autonomy, beneficence, and confidentiality are better positioned to comprehend the philosophical underpinnings of data protection.
Information privacy, on the other hand, extends beyond ethical obligation into the realm of legal enforcement. A Certified HIPAA Professional must understand not only what constitutes ethical behavior but also what is legally mandated. Foundational knowledge of privacy principles—data minimization, purpose limitation, and consent management—enables candidates to interpret HIPAA requirements with nuanced precision.
Additionally, comprehension of cybersecurity fundamentals enhances a professional’s ability to implement technical safeguards. Even though the CHP certification does not transform candidates into cybersecurity experts, it expects them to recognize the interdependencies between privacy policies and technological controls. Concepts such as encryption, access control, data classification, and incident response form part of the holistic knowledge base that supports effective HIPAA compliance.
Soft Skills and Cognitive Attributes That Elevate Performance
While technical and regulatory knowledge forms the backbone of HIPAA compliance, soft skills amplify its effectiveness. The ability to collaborate, lead, and adapt in dynamic environments is crucial for professionals managing privacy and security functions. A Certified HIPAA Professional often operates within cross-functional teams, requiring negotiation, diplomacy, and empathy.
Adaptability is another indispensable attribute. Healthcare environments are fluid, shaped by evolving technologies, regulations, and patient expectations. A CHP-certified professional must remain agile, able to adjust to new compliance frameworks or emerging security protocols. Adaptability also involves continuous learning—a willingness to revisit and refine one’s understanding as regulatory interpretations evolve.
Leadership, even in non-supervisory roles, is a subtle yet essential quality. The ability to inspire colleagues to embrace compliance as a collective responsibility distinguishes effective professionals from those who view it as a procedural burden. CHP candidates who exhibit initiative and accountability are better prepared to influence organizational culture positively.
Furthermore, emotional intelligence enhances a professional’s capacity to manage sensitive situations. Data breaches, privacy complaints, and ethical conflicts often require composed decision-making under pressure. A professional with high emotional intelligence can balance empathy for affected individuals with the analytical focus necessary for remediation and compliance reporting.
Preparing for Certification Without a Formal Background
Not all candidates pursuing the Certified HIPAA Professional credential originate from traditional healthcare or IT backgrounds. Some come from administrative, educational, or business sectors, drawn by the growing intersection of data privacy and organizational governance. For these individuals, strategic preparation can compensate for the absence of formal experience.
The first step involves familiarization with HIPAA’s structure and intent. Candidates can begin by studying publicly available resources that explain the Privacy and Security Rules in simplified terms. This helps establish a conceptual framework before delving into advanced study materials. Understanding terminology such as protected health information, covered entities, and business associates provides the linguistic foundation for more complex discussions.
Engaging in professional workshops or online courses focused on healthcare compliance can further enhance understanding. Many of these programs simulate real-world case studies, allowing candidates to explore hypothetical scenarios involving data breaches, risk assessments, and compliance audits. This experiential learning reinforces theoretical comprehension and builds confidence.
Networking with professionals in the healthcare or compliance domains also offers valuable insight. Informational interviews, mentorship programs, and professional associations allow aspiring candidates to learn from those already certified. This interaction not only broadens perspective but also clarifies the practical realities of HIPAA implementation in various organizational contexts.
Another effective preparation strategy involves developing interdisciplinary literacy. Candidates can study the basics of cybersecurity, organizational policy-making, and risk management, as these subjects frequently intersect with HIPAA compliance. Understanding how these domains overlap fosters a multidimensional approach to data protection—an essential trait for success in the certification examination and beyond.
Lastly, adopting a disciplined study routine enhances the chances of success. Consistency, rather than intensity, yields lasting comprehension. Allocating specific time blocks for studying regulatory concepts, reviewing case laws, and practicing situational analysis helps candidates internalize the material effectively. Supplementing study with practical exercises—such as drafting a mock privacy policy or analyzing a data breach scenario—transforms theoretical learning into applied expertise.
Why Prerequisites Matter in the Broader Context of Healthcare Compliance
Eligibility criteria and prerequisites are not arbitrary barriers; they exist to ensure that those entering the field of HIPAA compliance possess the cognitive maturity and ethical awareness necessary to handle the immense responsibility of patient privacy. The CHP certification is more than a testament to knowledge; it is a recognition of readiness. It signifies that the candidate can be trusted to operate in environments where errors have profound human and institutional consequences.
Healthcare organizations rely on CHP-certified professionals not only for regulatory adherence but also for guidance in shaping compliance strategies. These professionals interpret ambiguous regulations, anticipate emerging risks, and cultivate organizational cultures grounded in accountability. Their expertise ensures that compliance becomes a living practice rather than a static checklist.
Moreover, the prerequisites establish a benchmark of professionalism. They reflect a commitment to continuous learning and ethical responsibility—qualities indispensable in a discipline where legal, technological, and human considerations converge. A candidate who meets the eligibility standards demonstrates a dedication to the enduring principles of trust, confidentiality, and public welfare that define healthcare itself.
In essence, the prerequisites for the Certified HIPAA Professional certification are not merely procedural requirements but formative experiences. They nurture the intellectual dexterity, ethical conviction, and professional poise necessary to excel in the evolving landscape of healthcare privacy. Whether through education, experience, or self-directed growth, every aspiring professional undertakes a journey of transformation—one that refines their abilities and fortifies their role as guardians of patient trust in an age defined by information and vulnerability.
Exam Structure, Content, and Study Strategies for CHP Certification
The Certified HIPAA Professional certification is more than a conventional academic qualification; it represents an intricate assessment of one’s comprehension, judgment, and practical acumen in safeguarding healthcare privacy and ensuring adherence to regulatory frameworks. The certification examination functions as both a measure of professional readiness and a reflection of ethical commitment. Understanding the structure and substance of the examination, alongside effective preparation methodologies, forms the cornerstone of success for aspiring candidates. The path to certification demands more than rote memorization; it requires analytical precision, conceptual depth, and a disciplined strategy for assimilating and applying knowledge.
The CHP examination serves as a formalized evaluation of a candidate’s ability to interpret, apply, and manage the stipulations of the Health Insurance Portability and Accountability Act. It is meticulously designed to assess a professional’s aptitude in translating theoretical principles into practical compliance mechanisms that align with real-world healthcare operations. Each question is crafted to measure not only factual recall but also situational reasoning, ethical interpretation, and procedural insight. Candidates who understand the logic behind the exam’s structure can navigate it with confidence and discernment, rather than relying solely on memorization or superficial familiarity with terminology.
Understanding the Framework and Nature of the CHP Examination
The Certified HIPAA Professional examination generally encompasses multiple-choice and scenario-based questions that probe a candidate’s comprehension of HIPAA’s three principal rules: the Privacy Rule, the Security Rule, and the Breach Notification Rule. While the format may vary depending on the certifying institution, the underlying structure remains consistent in its emphasis on application-oriented learning. Each question is designed to evaluate how well the candidate can translate regulatory theory into functional compliance strategies.
The examination typically unfolds over a predetermined duration, testing both knowledge and time management. Candidates are required to balance precision with efficiency, as each question demands careful reading and analytical thought. The test structure is segmented into thematic domains that collectively represent the entire landscape of HIPAA compliance. These domains include regulatory fundamentals, administrative safeguards, technical controls, physical protection, and risk management. Within these areas, the examination integrates cross-disciplinary challenges that compel candidates to consider not only the legal obligations of compliance but also the ethical and operational implications of privacy protection in healthcare.
The Privacy Rule domain assesses understanding of how patient information must be collected, used, and disclosed within permissible boundaries. It tests comprehension of concepts such as minimum necessary standards, patient consent, and individual rights regarding access to personal health information. The Security Rule domain delves into the safeguards required to protect electronic protected health information, emphasizing access controls, audit mechanisms, encryption, and data integrity. Meanwhile, the Breach Notification Rule domain evaluates how candidates would identify, document, and report breaches, ensuring that appropriate corrective actions and disclosures are executed according to federal requirements.
Each domain interacts with the others, illustrating that HIPAA compliance operates as an integrated system rather than a collection of isolated regulations. The examination tests this integrative comprehension by presenting scenario-based questions that mimic real-life challenges, such as determining whether an incident qualifies as a reportable breach or designing a training protocol for new employees. A candidate’s ability to interpret the interrelationship between rules often determines the difference between average and exceptional performance.
Key Knowledge Areas and Cognitive Expectations
Mastery of HIPAA requires more than familiarity with legislative text. It calls for a multidimensional understanding that bridges law, technology, ethics, and organizational behavior. The CHP examination evaluates candidates across cognitive dimensions that include interpretation, analysis, synthesis, and evaluation. It demands that professionals not only know the statutes but comprehend the rationale behind them—why specific safeguards exist, how they protect patient interests, and what operational adjustments ensure compliance in different scenarios.
A core area of assessment is regulatory interpretation. Candidates must demonstrate the ability to translate complex legal language into actionable institutional policies. They may encounter questions that ask them to identify appropriate procedures in ambiguous situations or determine whether certain activities constitute violations under HIPAA standards. This evaluative thinking distinguishes true comprehension from mechanical recall.
Risk management and mitigation represent another critical area of focus. The examination expects candidates to identify vulnerabilities within healthcare systems, propose controls, and evaluate their effectiveness. This involves understanding risk assessment methodologies, such as identifying threats, assessing likelihood and impact, and prioritizing remediation efforts. Candidates must exhibit awareness of both technical and administrative countermeasures that maintain data confidentiality, integrity, and availability.
In addition, ethical awareness is interwoven throughout the examination. HIPAA’s mandates are not merely bureaucratic constructs; they stem from moral principles that safeguard the dignity and privacy of individuals. Questions may test the candidate’s ability to resolve ethical dilemmas, such as determining how to balance transparency with confidentiality or how to address noncompliance without compromising institutional harmony. Those who approach the examination with an ethical mindset often perform better, as they understand that compliance transcends regulation—it reflects moral stewardship.
Strategies for Effective Preparation and Study Discipline
Preparing for the CHP certification examination demands strategic planning and intellectual discipline. Random or unstructured study often leads to fragmented understanding. A systematic approach, integrating both theoretical review and applied learning, enhances retention and comprehension.
An initial step in preparation involves familiarizing oneself with the complete body of HIPAA regulations, including the Privacy, Security, and Breach Notification Rules. Candidates should read official documentation issued by the U.S. Department of Health and Human Services, as it offers authoritative explanations and examples of regulatory interpretation. Engaging with case studies where organizations have faced penalties or corrective actions provides tangible insights into compliance failures and corrective mechanisms.
Creating a structured study plan enables candidates to allocate sufficient time to each knowledge domain. The schedule should incorporate incremental learning, where each concept builds upon the previous one. Instead of memorizing regulations verbatim, candidates should focus on understanding their practical application. Reviewing real-world incidents, such as data breaches or compliance audits, helps contextualize theoretical principles.
Practice tests play an instrumental role in preparation. They acquaint candidates with question formats and time constraints, revealing areas that require further study. Reviewing incorrect answers is particularly beneficial, as it exposes misconceptions and strengthens conceptual clarity. Candidates should approach practice exams not as mere drills but as diagnostic tools that refine analytical reasoning.
Collaborative learning also enhances comprehension. Discussing regulatory interpretations with peers, joining professional study groups, or attending preparatory workshops allows candidates to exchange perspectives and clarify ambiguities. Explaining a concept to others reinforces personal understanding, converting abstract knowledge into articulate expression—a skill invaluable during the actual examination.
In addition to technical preparation, mental readiness holds equal significance. Time management, focus, and composure play crucial roles during the test. Candidates should practice pacing themselves, allotting consistent time per question while leaving room for review. Regular study breaks, adequate rest, and mindfulness techniques help sustain concentration during the lengthy preparation period.
Unconventional Study Approaches for Distinct Mastery
While traditional study methods provide the foundation, unconventional techniques can yield distinctive advantages. Visualization is one such approach—transforming textual regulations into conceptual diagrams or mental models that illustrate relationships between HIPAA’s various rules. For instance, mapping how administrative safeguards correspond to technical controls enhances the ability to recall and apply them contextually.
Analogical learning also proves powerful. Comparing HIPAA compliance structures with familiar systems—such as financial risk management or corporate governance—helps assimilate abstract regulatory concepts. These analogies simplify complex ideas and embed them in long-term memory through association.
Another uncommon yet effective strategy is scenario reconstruction. Candidates can imagine themselves as compliance officers handling specific incidents, such as an unauthorized access attempt or an employee’s accidental disclosure of patient information. By drafting hypothetical response plans, they develop procedural intuition and adaptive thinking. This method transcends theoretical learning, fostering the capacity to act decisively under pressure.
Integrating micro-learning techniques further refines comprehension. Instead of extended study sessions, candidates can break material into digestible segments and review them periodically. This technique exploits the brain’s natural retention patterns, ensuring steady accumulation of knowledge without fatigue. Incorporating auditory learning through recorded lectures or self-narration reinforces familiarity with key terms and concepts.
Additionally, reflective journaling can transform study into introspection. After each session, writing a brief summary of what was learned and identifying how it connects to professional experiences deepens understanding. Reflection converts passive study into active cognition, strengthening conceptual frameworks essential for complex reasoning tasks on the examination.
Navigating Common Pitfalls and Cognitive Barriers
The path to CHP certification, though intellectually rewarding, can be fraught with challenges. Many candidates falter not due to lack of knowledge but because of inadequate preparation strategies or cognitive missteps. Recognizing and mitigating these pitfalls is integral to ensuring success.
One prevalent error involves overreliance on memorization. While recalling specific regulations is necessary, the examination predominantly assesses application. Candidates who focus solely on rote learning often struggle to interpret questions framed within practical scenarios. The remedy lies in contextual learning—understanding why a rule exists and how it governs specific behaviors or institutional processes.
Another frequent obstacle is underestimating the interdisciplinary nature of HIPAA. Some candidates approach the examination with a purely legal or technical mindset, neglecting the ethical and administrative dimensions. Effective preparation requires a holistic perspective that unites all aspects of compliance—policy, technology, ethics, and governance—into a cohesive understanding.
Time mismanagement during the test also proves detrimental. Spending disproportionate time on complex questions can lead to rushed responses later. Developing pacing strategies during practice exams mitigates this risk. Candidates should learn to identify and address easier questions first, returning to more demanding ones afterward.
Emotional fatigue and test anxiety can impair performance. Maintaining psychological equilibrium through regular rest, balanced nutrition, and relaxation techniques improves concentration and recall. Visualization exercises—imagining success or rehearsing calm responses to difficult questions—train the mind to remain composed under pressure.
Additionally, neglecting to review updates to HIPAA regulations or enforcement interpretations can hinder performance. The healthcare regulatory landscape evolves, and the examination may reflect contemporary developments. Staying informed through credible industry publications and compliance bulletins ensures candidates remain attuned to current standards.
Time Management and Performance Optimization
Mastering time allocation is a decisive factor in achieving success. Each question must be approached with balance—thorough analysis without unnecessary hesitation. A common strategy involves allotting a specific number of minutes per question based on total exam time, leaving a reserve period for review.
During the test, reading comprehension is paramount. Misinterpreting question phrasing can lead to avoidable errors. Candidates should read each question carefully, identify the central issue, and eliminate distractors before selecting the answer that aligns most closely with regulatory logic. In scenario-based items, recognizing the intent behind the situation—such as whether it emphasizes ethical decision-making or procedural accuracy—guides effective judgment.
Maintaining steady cognitive rhythm prevents burnout. Short mental resets, such as deep breathing or brief visualization, can restore focus. Candidates must remember that the examination rewards consistent reasoning more than impulsive certainty. Even if an answer seems uncertain, logical elimination of incorrect options increases accuracy.
Finally, reviewing responses with fresh perspective can uncover overlooked nuances. Revisiting questions after completing the test often yields corrections that refine the overall score. The ability to self-assess calmly and methodically distinguishes successful candidates from those who succumb to haste or anxiety.
Integrating Preparation into Professional Identity
Preparing for the Certified HIPAA Professional certification is not merely an academic pursuit—it represents an evolution of professional identity. Candidates who approach the process as a journey of intellectual refinement and ethical maturity derive enduring value beyond the examination itself. The study of HIPAA regulations invites reflection on the broader principles of trust, integrity, and accountability that underpin healthcare.
Through disciplined preparation, candidates internalize the ethos of compliance as a moral commitment rather than a bureaucratic obligation. This transformation manifests in daily professional conduct—how they handle confidential information, communicate with colleagues, and respond to ethical dilemmas. The certification thus becomes not just a symbol of expertise but a declaration of professional conscience.
In an era where data breaches and privacy violations can undermine institutional credibility, the knowledge and judgment acquired through CHP certification preparation equip professionals to act as custodians of public trust. Every hour of study, every practice question, and every reflection upon regulatory principles contributes to a deeper understanding of the sacred relationship between healthcare providers and the individuals they serve.
The examination, therefore, is not merely a test of information but a rite of passage into a community of professionals dedicated to preserving the sanctity of health information. Through diligence, self-awareness, and intellectual curiosity, candidates emerge not only as certified experts but as enlightened advocates for ethical data stewardship in the ever-evolving realm of healthcare privacy.
Understanding the Core Functions of a Certified HIPAA Professional in the Modern Healthcare Landscape
In the intricate ecosystem of healthcare, where patient information traverses through digital channels and administrative workflows, the role of a Certified HIPAA Professional (CHP) becomes an indispensable pillar of trust, compliance, and security. A CHP-certified individual is not merely a regulatory gatekeeper; they are the sentinels of data sanctity, ensuring that every byte of sensitive patient information remains protected under the strict provisions of the Health Insurance Portability and Accountability Act (HIPAA). Their multifaceted responsibilities span across policy implementation, staff training, risk analysis, and breach management, all of which collectively safeguard an organization’s ethical and operational integrity.
A Certified HIPAA Professional functions as the linchpin between regulatory compliance and practical healthcare operations. Their daily obligations are rooted in the preservation of privacy, but their influence extends into shaping a culture of confidentiality within hospitals, clinics, insurance entities, and healthcare technology firms. They are tasked with transforming abstract legal statutes into actionable policies that medical staff, IT administrators, and executives can seamlessly adhere to. This transformation requires both analytical acuity and empathetic understanding, as they must balance the rigor of legal obligations with the human dimensions of healthcare service delivery.
One of the principal duties of a Certified HIPAA Professional involves conducting in-depth privacy and security audits. These audits are not perfunctory reviews but rather comprehensive evaluations of how an organization manages protected health information (PHI). The CHP must assess data flow, access control mechanisms, physical safeguards, and electronic system vulnerabilities. Each audit involves meticulous scrutiny, identifying discrepancies between written policies and operational realities. For instance, a CHP may examine how electronic health record systems are accessed and whether permissions are configured according to the principle of least privilege. In doing so, they ensure that only authorized personnel have access to patient data relevant to their responsibilities, minimizing the risk of unauthorized exposure.
Beyond audits, risk assessment is another cornerstone of the CHP’s responsibilities. This entails identifying potential vulnerabilities in information systems and administrative protocols that could jeopardize data confidentiality or integrity. These assessments are both proactive and reactive. Proactively, the CHP anticipates possible threats—such as phishing attacks, weak authentication measures, or outdated encryption protocols—and formulates strategies to counter them. Reactively, they evaluate past incidents to prevent recurrence, learning from security breaches or near misses. A robust risk management program led by a CHP often determines how well an organization withstands regulatory scrutiny or public trust challenges in the aftermath of a breach.
Another vital role of a CHP-certified professional is the development and implementation of privacy and security policies. These documents serve as the backbone of organizational compliance, translating federal regulations into actionable internal standards. A Certified HIPAA Professional must ensure these policies are both legally sound and operationally feasible. This often involves collaboration with multiple departments—IT, legal, clinical, and human resources—to align regulatory requirements with workflow realities. For instance, while legal advisors interpret the legislative text of HIPAA, the CHP ensures that these interpretations manifest effectively in technical and administrative practices.
Training and education represent a fundamental aspect of a CHP’s portfolio. HIPAA compliance is not achieved through documentation alone; it thrives through awareness and adherence. A CHP-certified professional designs and delivers training programs tailored to different staff levels within an organization. These sessions may include orientations for new employees, refresher courses for existing staff, and specialized workshops for high-risk departments such as billing or IT. Training content typically covers topics such as recognizing phishing emails, managing password hygiene, handling paper records securely, and reporting potential data breaches. By fostering a culture of vigilance, the CHP helps instill a sense of collective responsibility across all tiers of an organization.
When a breach occurs—a possibility even within the most vigilant systems—the CHP assumes a central role in managing the response. Their tasks begin with identifying and containing the breach, determining its scope, and assessing which patient records or systems were affected. They then guide the organization through the reporting process, ensuring compliance with the HIPAA Breach Notification Rule, which mandates timely communication to affected individuals, the Department of Health and Human Services (HHS), and sometimes the media. This phase demands exceptional composure and procedural precision, as any misstep can exacerbate legal liabilities or reputational harm.
A Certified HIPAA Professional must also collaborate closely with IT departments to ensure that technical safeguards align with regulatory standards. This collaboration might involve overseeing encryption practices, firewall configurations, intrusion detection systems, and access control frameworks. They work with cybersecurity teams to establish secure data transmission channels, both internally and externally, ensuring that patient information shared between entities—such as hospitals, insurance providers, or laboratories—remains uncompromised. Moreover, the CHP monitors emerging technologies such as telehealth systems and mobile health applications, assessing their compliance with HIPAA’s privacy and security provisions.
Documentation and recordkeeping are equally critical to a CHP’s duties. Every audit, training session, risk analysis, and breach response must be documented thoroughly. This meticulous recordkeeping is not mere bureaucracy; it serves as evidence of due diligence in the event of regulatory investigations. When the Office for Civil Rights (OCR) conducts an audit or responds to a complaint, these records demonstrate that the organization has established and maintained compliance measures in good faith. A well-documented compliance program often mitigates penalties even in cases of inadvertent noncompliance, highlighting the strategic importance of administrative precision.
Ethical considerations permeate every aspect of a CHP’s work. While HIPAA provides a legal framework, the moral foundation of healthcare privacy rests on respect for patient autonomy and dignity. A Certified HIPAA Professional must navigate delicate ethical terrains where operational necessity intersects with individual rights. For example, in emergency situations where patient information must be disclosed to ensure timely care, the CHP ensures such disclosures adhere strictly to the “minimum necessary” standard, preventing overexposure of sensitive data. Similarly, they counsel staff on the ethical handling of incidental disclosures—unintentional breaches that may occur in everyday clinical settings. Their guidance ensures that privacy is not treated as a procedural formality but as a moral obligation intrinsic to the ethos of healthcare.
In addition to internal responsibilities, CHP professionals frequently act as liaisons with external entities such as regulatory bodies, business associates, and third-party vendors. This involves negotiating and maintaining Business Associate Agreements (BAAs), which outline how external partners handle protected health information. The CHP ensures that these agreements meet HIPAA standards and that partners uphold equivalent levels of data protection. With the increasing complexity of digital ecosystems and outsourcing in healthcare, managing vendor compliance has become a critical and challenging responsibility.
Incident response planning constitutes another dimension of a CHP’s function. While it overlaps with breach management, incident response encompasses broader preparation for potential security threats. The CHP helps design response plans that specify roles, communication channels, escalation protocols, and recovery procedures. Regular simulations or “tabletop exercises” are conducted under their guidance to test organizational readiness for data breaches, ransomware attacks, or system failures. These proactive rehearsals ensure that, when a real incident occurs, the organization can respond swiftly and cohesively, minimizing both operational disruption and regulatory risk.
Another area of involvement for a Certified HIPAA Professional is in continuous improvement and monitoring. Compliance is not static; it evolves with changes in law, technology, and organizational structure. A CHP must stay abreast of amendments to HIPAA, related regulations such as HITECH (Health Information Technology for Economic and Clinical Health Act), and new guidance from oversight agencies. They interpret these changes and integrate them into existing compliance programs, ensuring the organization remains perpetually aligned with the current regulatory landscape.
Beyond compliance, CHPs play a strategic role in cultivating trust—an invaluable asset in healthcare. Patients entrust their most intimate information to healthcare providers, believing it will remain confidential. A Certified HIPAA Professional reinforces that trust by ensuring transparency in data handling practices and consistency in privacy enforcement. Their presence within an organization signals to both patients and regulators that data protection is not merely a checkbox activity but a foundational principle guiding every operation.
In larger healthcare institutions, a CHP may lead a team of privacy officers, compliance analysts, and IT security personnel. Leadership in this capacity demands both technical literacy and interpersonal dexterity. They must inspire compliance not through coercion but through education and example. By demonstrating the tangible impact of privacy protection—both in safeguarding patients and preserving organizational integrity—they cultivate an environment where compliance becomes an intrinsic value shared by all employees.
The CHP’s expertise also extends into policy advocacy and advisory roles. They may contribute to internal governance boards, advising on data-sharing initiatives, clinical research protocols, or digital transformation projects. Their perspective ensures that innovation does not outpace compliance, enabling organizations to adopt new technologies responsibly. For example, as healthcare increasingly embraces artificial intelligence and predictive analytics, a CHP assesses the privacy implications of these tools, ensuring that algorithms and datasets adhere to de-identification and consent requirements.
Moreover, a Certified HIPAA Professional plays a critical role in shaping communication protocols within healthcare organizations. They oversee how patient information is shared through email, fax, cloud systems, or mobile devices, establishing guidelines that balance efficiency with security. The rise of telemedicine and remote work arrangements has further complicated this landscape, requiring CHPs to implement advanced encryption standards, secure communication platforms, and multifactor authentication mechanisms for remote access. Their vigilance ensures that the convenience of digital healthcare never compromises patient confidentiality.
In the realm of compliance auditing, CHPs may also interact with external auditors or accreditation bodies to verify adherence to not just HIPAA, but complementary frameworks like ISO 27001 or NIST cybersecurity standards. Their cross-disciplinary understanding allows them to harmonize HIPAA compliance with broader information security objectives, thereby enhancing organizational resilience. This harmonization is crucial in a globalized healthcare environment where data often crosses geographical and jurisdictional boundaries.
Lastly, continuous self-education defines the ethos of a Certified HIPAA Professional. Healthcare technology and privacy threats evolve incessantly, and complacency is an adversary to compliance. A CHP invests in ongoing learning through professional development courses, privacy law seminars, and participation in industry conferences. This pursuit of perpetual knowledge equips them to anticipate regulatory shifts and technological trends before they crystallize into operational challenges.
In essence, the responsibilities of a Certified HIPAA Professional transcend the boundaries of compliance checklists. They embody the convergence of law, ethics, and technology in healthcare. Their work safeguards not only data but also the trust that forms the very foundation of the patient-provider relationship. Through their diligence, foresight, and commitment to ethical stewardship, they fortify the invisible infrastructure upon which the integrity of modern healthcare securely rests.
Exploring Professional Growth, Leadership, and Opportunities for Certified HIPAA Professionals
The Certified HIPAA Professional certification has become a defining credential for individuals aiming to advance their careers within healthcare privacy, compliance, and data protection. In a world where healthcare information is increasingly digitized, and where patient confidentiality is not just a legal obligation but an ethical cornerstone, this certification represents both a badge of competence and a passport to professional ascension. The healthcare sector, being vast and multidimensional, requires professionals who can navigate the intricacies of compliance, technology, and human behavior with equal finesse. Earning the CHP certification thus opens numerous pathways to career advancement, enhanced credibility, and leadership opportunities across clinical, administrative, and technological domains.
For many professionals, the pursuit of CHP certification begins with a fundamental aspiration: to gain authority and expertise in the realm of healthcare data privacy. Once certified, however, individuals often discover that its impact reverberates far beyond compliance documentation or risk management tasks. The CHP credential is a marker of trustworthiness and mastery—attributes that healthcare employers deeply value. Whether one works as a compliance officer, information security analyst, clinical manager, or policy consultant, the certification positions its holder as a dependable guardian of patient data integrity and institutional reputation.
Career advancement for Certified HIPAA Professionals is anchored in a growing demand for specialized knowledge. With increasing cyber threats, evolving federal regulations, and expanding data-sharing initiatives, organizations are in constant need of experts who can translate complex regulatory frameworks into actionable strategies. Hospitals, insurance companies, government agencies, and health technology vendors all require individuals who can ensure that their data-handling practices remain compliant with HIPAA. A CHP-certified professional is uniquely qualified to fill this role, offering both legal literacy and operational insight. This dual competency allows them to bridge communication gaps between legal teams, IT departments, and executive leadership—an invaluable skill that often propels them into managerial or strategic positions.
The financial benefits of obtaining CHP certification are equally compelling. Professionals holding this credential often witness salary increments and broader job mobility. As compliance-related responsibilities carry high stakes, organizations are willing to compensate those who can mitigate legal risk and protect institutional integrity. Beyond monetary gain, however, there is a profound sense of professional validation that accompanies certification. It symbolizes a commitment to ongoing learning and an ethical approach to patient data protection, qualities that resonate deeply within the healthcare community. In many organizations, Certified HIPAA Professionals are entrusted with overseeing privacy initiatives, leading cross-departmental compliance teams, and mentoring staff, thereby cementing their influence within the organizational hierarchy.
The journey of career advancement after earning CHP certification also involves expanding one’s professional scope. Many certified individuals diversify their roles by integrating their HIPAA expertise with other disciplines such as cybersecurity, risk management, healthcare administration, or data governance. For instance, a professional who begins as a compliance specialist may evolve into a Chief Privacy Officer or Director of Information Governance, guiding institutional policy and long-term strategic vision. Similarly, those with technical backgrounds may progress into cybersecurity leadership roles, using their CHP foundation to ensure that security protocols align with regulatory mandates. This cross-functional adaptability makes the CHP credential not just a qualification but a springboard for lifelong career evolution.
Networking forms another vital pillar of career growth for Certified HIPAA Professionals. Building connections within the compliance and healthcare communities can open doors to new opportunities, collaborations, and mentorship. Professionals often engage in associations such as the Health Care Compliance Association (HCCA) or attend conferences on privacy and data security to stay abreast of emerging issues. These engagements not only broaden knowledge but also enhance visibility among peers and potential employers. Through networking, CHPs gain access to policy discussions, industry innovations, and evolving compliance interpretations, which collectively enrich their professional competence and relevance.
Continuous education plays an equally transformative role in sustaining career momentum. The healthcare landscape evolves relentlessly, shaped by new technologies, telemedicine platforms, and evolving federal mandates. A Certified HIPAA Professional who remains intellectually agile—participating in advanced training, webinars, and specialized certifications—retains an edge in this competitive domain. Expanding knowledge beyond HIPAA, such as exploring the Health Information Technology for Economic and Clinical Health (HITECH) Act, GDPR, or ISO standards, strengthens a professional’s ability to navigate both domestic and global data privacy ecosystems. Such intellectual breadth not only deepens expertise but also demonstrates a proactive commitment to excellence, a trait that employers consistently seek in leadership candidates.
Another dimension of career advancement lies in the development of soft skills that complement technical acumen. While a CHP certification validates one’s regulatory understanding, leadership success often depends on communication, negotiation, and ethical decision-making. Certified HIPAA Professionals frequently find themselves mediating between compliance requirements and operational demands, necessitating persuasive communication and diplomacy. They must articulate complex legal concepts in accessible terms for non-technical staff, resolve privacy disputes with discretion, and guide organizations through regulatory audits without friction. Mastering these interpersonal dimensions transforms a technically competent individual into an influential leader capable of inspiring compliance-minded cultures across entire institutions.
Leadership opportunities for CHP-certified individuals have expanded remarkably in recent years. Healthcare organizations increasingly recognize that compliance leadership is not a peripheral function but a strategic one. As a result, many institutions are elevating privacy professionals to executive roles, such as Chief Compliance Officer or Chief Privacy Officer. These positions involve not just enforcing policies but designing institutional frameworks that balance patient rights with organizational innovation. Certified HIPAA Professionals, with their holistic understanding of legal, ethical, and operational principles, are ideally suited to assume these high-level responsibilities. Their influence extends to policymaking, technological procurement, vendor management, and crisis communication—areas that define the organization’s public reputation and regulatory standing.
For those inclined toward consultancy or entrepreneurship, the CHP certification can serve as a powerful credential for establishing independent practices. Many professionals leverage their expertise to advise healthcare startups, clinics, or technology companies developing digital health platforms. Their guidance ensures that emerging products and services comply with privacy regulations from inception. This consulting path not only offers financial autonomy but also intellectual gratification, as consultants often work on diverse projects ranging from policy formulation to risk assessment and breach mitigation. Moreover, as healthcare data exchange expands through interoperable systems and cloud-based solutions, demand for HIPAA consulting services is expected to grow exponentially, further enhancing the career potential for certified experts.
In academia and training, Certified HIPAA Professionals find rewarding opportunities to impart their knowledge to the next generation of compliance and healthcare specialists. By serving as lecturers, trainers, or curriculum developers, they contribute to shaping institutional awareness around patient privacy and ethical data use. Their firsthand experience enriches educational programs, translating theoretical HIPAA provisions into real-world scenarios that students and professionals can readily grasp. In doing so, they not only advance their careers but also uphold a collective commitment to ethical stewardship within the healthcare industry.
The CHP certification also enhances cross-industry mobility. While it is primarily rooted in healthcare, the principles of privacy, risk management, and data governance are universally applicable across sectors such as insurance, pharmaceuticals, public health administration, and health technology development. Professionals can therefore transition into diverse environments where their expertise remains indispensable. For example, a CHP-certified professional might move from a hospital compliance office to a health insurance firm’s data privacy division or a biotechnology company developing patient data solutions. This adaptability expands career horizons and protects professionals from the volatility of industry-specific changes.
An often-overlooked advantage of CHP certification lies in its contribution to professional reputation and credibility. Employers and colleagues view certified individuals as reliable authorities in compliance matters, often turning to them for strategic input on complex privacy dilemmas. This perception of reliability fosters not only career growth but also personal fulfillment, as professionals recognize the tangible impact of their expertise on patient safety and organizational trust. Over time, this credibility evolves into influence, empowering CHPs to shape institutional ethics, policies, and operational philosophies that prioritize transparency and accountability.
Career advancement for Certified HIPAA Professionals also hinges on the ability to adapt to digital transformation within healthcare. As artificial intelligence, big data analytics, and telemedicine redefine how patient information is collected and utilized, CHP-certified individuals must ensure that compliance frameworks evolve in tandem. This may involve collaborating with developers to integrate privacy-by-design principles into software systems, overseeing consent management for data analytics, or evaluating cloud-based solutions for compliance alignment. Their strategic foresight ensures that innovation does not outpace regulation, maintaining the delicate equilibrium between technological progress and ethical responsibility.
Many Certified HIPAA Professionals eventually find their way into policy advisory or governmental roles. Their in-depth understanding of HIPAA positions them as valuable contributors to legislative consultations, compliance task forces, and public policy development. In such capacities, they influence how future regulations are shaped, ensuring that laws remain practical, relevant, and attuned to the evolving realities of healthcare. Engaging at this level of governance offers profound career enrichment, as professionals transition from compliance implementers to policy architects shaping the very frameworks they once enforced.
Within healthcare organizations, a Certified HIPAA Professional’s career trajectory often includes involvement in interdisciplinary projects. They may collaborate with clinical informatics teams, research boards, and technology developers to evaluate privacy implications of new systems or research initiatives. This exposure broadens their professional perspective, equipping them to manage projects that require balancing scientific innovation with privacy safeguards. Over time, such cross-departmental collaborations can pave the way for strategic leadership roles, where the professional becomes instrumental in guiding institutional transformation toward both innovation and integrity.
The impact of CHP certification on professional development is not limited to organizational advancement; it also fosters personal growth. The process of mastering HIPAA regulations, interpreting evolving case laws, and handling real-world privacy challenges sharpens analytical thinking and decision-making acumen. These intellectual attributes are transferable across professional domains, enhancing resilience and adaptability. Moreover, the ethical foundation of HIPAA compliance instills a profound sense of purpose. Many Certified HIPAA Professionals find deep satisfaction in knowing that their work protects not just data, but human dignity—a value that transcends career ambition.
For professionals aiming to enhance their career trajectory further, pursuing additional credentials that complement CHP certification can be advantageous. Certifications in risk management, cybersecurity, or healthcare management—such as CISSP, CHPS, or CPHIMS—can fortify one’s professional profile. When combined, these qualifications create a multidimensional expertise that is rare and highly sought after. Employers increasingly prefer candidates who can synthesize technical security measures with regulatory acumen and business strategy, making such combinations a powerful formula for leadership success.
The evolution of healthcare toward data-driven decision-making further amplifies the relevance of Certified HIPAA Professionals. As organizations harness patient data for analytics, research, and population health initiatives, privacy professionals become integral to ensuring ethical and legal data use. CHPs guide these initiatives by establishing frameworks that protect personal information while allowing data utility for improving healthcare outcomes. This delicate balance requires a blend of legal understanding, technological literacy, and ethical reasoning—skills honed through rigorous CHP training and experience.
Ultimately, career advancement for Certified HIPAA Professionals is an ongoing odyssey characterized by learning, leadership, and adaptation. The certification does not represent an endpoint but a foundation upon which a lifelong pursuit of excellence is built. Each role, project, and collaboration expands their influence within the healthcare continuum. Their work transcends organizational confines, shaping an industry that aspires not only to cure and care but also to respect and protect. Through diligence, foresight, and ethical conviction, CHP-certified individuals ascend from compliance specialists to visionary leaders—custodians of privacy in an era where trust has become the most valuable currency in healthcare.
Sustaining Professional Excellence and Navigating the Evolving Landscape of Healthcare Privacy
The Certified HIPAA Professional certification embodies a continuous commitment to mastery, ethical integrity, and adaptive learning. In an environment where healthcare regulations and technologies evolve ceaselessly, maintaining one’s CHP certification is not merely a procedural requirement but a vital component of professional resilience and credibility. The healthcare sector’s rapid digital transformation, coupled with escalating cybersecurity threats, has made the role of a Certified HIPAA Professional more dynamic and consequential than ever. To remain relevant and authoritative, professionals must engage in perpetual education, renew their certification periodically, and cultivate a forward-looking mindset attuned to the subtle shifts within privacy legislation and healthcare operations.
Maintaining the certification requires more than the passive accumulation of credits or completion of annual training. It demands an active commitment to intellectual agility, vigilance against regulatory changes, and participation in a broader professional discourse surrounding data privacy. For many Certified HIPAA Professionals, the renewal process becomes an opportunity for introspection—an assessment of one’s evolving competencies, ethical standards, and professional influence within the healthcare ecosystem. Renewal signifies that a professional not only retains technical and regulatory expertise but also evolves in tandem with an ever-changing legal and technological climate.
A crucial component of maintaining the certification lies in understanding the formal continuing education requirements. Certification authorities typically mandate that professionals complete a specific number of continuing education units (CEUs) or equivalent learning hours within a defined period. These can be earned through professional workshops, privacy seminars, accredited courses, or participation in conferences dedicated to healthcare compliance. However, the true value of these engagements extends beyond satisfying formal criteria—they offer Certified HIPAA Professionals the opportunity to interact with peers, learn about emerging technologies, and gain insight into the practical implications of regulatory updates. Networking through such educational platforms often leads to intellectual enrichment, mentorship opportunities, and collaborative problem-solving that amplify a professional’s effectiveness in the workplace.
Staying updated with HIPAA changes requires a deep awareness of how federal and state-level regulations intersect. While HIPAA forms the bedrock of healthcare privacy law in the United States, supplemental legislation such as the Health Information Technology for Economic and Clinical Health Act (HITECH) and various state-specific privacy laws continually shape the compliance landscape. Certified HIPAA Professionals must remain vigilant to ensure that their organizations comply not only with federal requirements but also with local laws governing patient information, data retention, and electronic health record systems. They often subscribe to legal briefings, attend government webinars, and engage with compliance newsletters to stay abreast of amendments, enforcement actions, and interpretive guidance issued by the Department of Health and Human Services (HHS).
In addition to monitoring legal updates, Certified HIPAA Professionals must cultivate an acute understanding of technological developments that impact data security and privacy. The healthcare industry is increasingly adopting cloud computing, artificial intelligence, wearable technology, and telehealth platforms—all of which introduce new vectors of risk. To maintain certification effectively, professionals must not only understand the theoretical aspects of compliance but also develop practical literacy in these technologies. They must discern how encryption standards evolve, how data sharing protocols are implemented, and how new devices interface with protected health information (PHI). This dual fluency—legal and technical—is the hallmark of a truly competent and forward-thinking CHP-certified professional.
The maintenance of certification also involves institutional participation. Many Certified HIPAA Professionals assume leadership roles in compliance committees, audit boards, or data governance councils within their organizations. Through these roles, they stay actively engaged in applying HIPAA principles in real-world contexts. Participation in such forums strengthens their ability to interpret new regulations pragmatically, ensuring that compliance strategies are both effective and adaptable. Furthermore, institutional involvement fosters a culture of collective responsibility, where every member of the healthcare team—from administrative assistants to IT engineers—understands and embraces the principles of confidentiality and ethical data handling.
Ethical consistency is another pillar of maintaining one’s certification. While laws may evolve, the moral imperatives of privacy remain immutable. Certified HIPAA Professionals are custodians of patient dignity and confidentiality, and their continued certification signifies ongoing dedication to these values. To sustain professional integrity, CHPs must navigate ethical dilemmas with discernment, balancing organizational demands with the inviolable rights of patients. This often involves making challenging decisions—such as reporting potential violations, addressing negligence, or resisting pressure to compromise privacy for expediency. Upholding ethical fidelity not only reinforces one’s credibility but also enhances the public trust that underpins the entire healthcare system.
The process of staying updated with HIPAA also entails an understanding of enforcement trends. The Office for Civil Rights (OCR), which oversees HIPAA compliance, periodically updates its focus areas based on prevalent risks or emerging patterns of noncompliance. For instance, recent years have seen intensified scrutiny of ransomware preparedness, risk analysis procedures, and business associate agreements. Certified HIPAA Professionals must anticipate such regulatory priorities and prepare their organizations accordingly. By studying past enforcement cases and penalties, they can identify common pitfalls and implement preemptive measures to mitigate risk. This proactive stance not only strengthens organizational resilience but also underscores the professional foresight that defines a seasoned compliance expert.
Digital literacy and cybersecurity competence have become indispensable for maintaining relevance as a Certified HIPAA Professional. With the proliferation of sophisticated cyberattacks targeting healthcare systems, CHPs must collaborate with IT departments to fortify data protection measures. Continuous training in cybersecurity principles—such as zero-trust architecture, multifactor authentication, and secure cloud frameworks—ensures that compliance remains robust even in the face of technological disruption. Many professionals pursue additional certifications in cybersecurity or risk management to complement their CHP credential, thereby enhancing their capacity to lead interdisciplinary efforts aimed at safeguarding patient data in both physical and digital environments.
Regular engagement with professional communities also enriches the certification maintenance journey. By participating in online forums, discussion groups, or professional associations dedicated to healthcare compliance, Certified HIPAA Professionals gain exposure to diverse perspectives and problem-solving methodologies. These exchanges often illuminate practical solutions to complex issues—such as cross-border data sharing, vendor risk management, or ethical AI deployment in healthcare. Moreover, such communities foster mentorship and peer learning, which are invaluable for both newly certified professionals and experienced practitioners seeking to refine their expertise. In this way, maintaining certification becomes not an isolated obligation but a shared endeavor rooted in communal growth and professional solidarity.
The ability to interpret and apply updates to HIPAA regulations distinguishes an exemplary Certified HIPAA Professional from a merely credentialed one. When new guidelines are introduced, professionals must conduct thorough analyses to assess their implications for organizational policies and procedures. This may involve revising privacy notices, updating risk management frameworks, or reconfiguring access control systems. The CHP serves as both analyst and strategist, ensuring that compliance adaptations occur seamlessly without disrupting operational continuity. This analytical rigor transforms the act of staying updated into a form of strategic leadership, wherein the Certified HIPAA Professional becomes a key architect of organizational resilience.
Another essential practice for maintaining certification is self-assessment. Periodic reflection on one’s knowledge gaps, procedural effectiveness, and ethical conduct fosters a mindset of continuous improvement. Certified HIPAA Professionals who conduct regular self-audits or solicit feedback from colleagues often discover opportunities for growth that formal training may not reveal. Such introspection cultivates humility and adaptability—qualities that are increasingly prized in a profession that straddles the intersection of law, technology, and human welfare.
In the broader context of healthcare evolution, maintaining CHP certification ensures that professionals remain integral contributors to institutional innovation. As healthcare transitions toward interoperability, data analytics, and patient-centric care models, privacy professionals must guide organizations in integrating these advancements responsibly. Their ability to interpret regulatory updates and align them with technological innovation safeguards both compliance and ethical integrity. By maintaining their certification, CHPs reaffirm their role as navigators of ethical progress—ensuring that healthcare modernization never undermines the sanctity of patient trust.
The renewal process also symbolizes professional accountability. By adhering to continuing education and renewal requirements, Certified HIPAA Professionals demonstrate their dedication to excellence and transparency. This accountability extends beyond regulatory expectations; it reflects a deeper acknowledgment of their duty to the public. In an age when data breaches and misinformation can erode confidence in healthcare systems, such accountability becomes a moral imperative as much as a professional one. Each renewal cycle, therefore, is not a routine administrative task but a reaffirmation of the professional’s commitment to uphold the highest standards of privacy, diligence, and compassion.
Technological adaptation represents a continuing frontier in the maintenance of certification. Emerging paradigms such as blockchain for medical records, machine learning for diagnostics, and global interoperability standards are reshaping how patient information is stored, analyzed, and exchanged. Certified HIPAA Professionals must not only comprehend these innovations but also anticipate their regulatory ramifications. They play a critical role in ensuring that the deployment of new technologies respects both legal frameworks and ethical boundaries. By staying educated on these developments, CHPs help steer healthcare institutions toward modernization that harmonizes innovation with integrity.
International perspectives on data protection also enhance the expertise of Certified HIPAA Professionals. Although HIPAA is an American law, global privacy regulations such as the General Data Protection Regulation (GDPR) influence best practices worldwide. Understanding these frameworks equips professionals to manage data in multinational healthcare organizations or research collaborations that transcend national borders. Integrating global privacy principles with HIPAA compliance demonstrates intellectual versatility and positions the CHP as a globally competent professional capable of navigating diverse regulatory landscapes.
Institutional collaboration remains one of the most effective ways to sustain professional growth and relevance. Certified HIPAA Professionals who mentor junior compliance officers or participate in cross-departmental training contribute not only to their own learning but also to organizational maturity. Mentorship reinforces knowledge retention and fosters leadership qualities, while collaborative projects encourage the exchange of diverse perspectives essential for adaptive problem-solving. In many cases, such engagement leads to recognition within professional circles, further strengthening the individual’s reputation as a trusted authority in healthcare privacy.
Renewal also entails vigilance in documentation. Maintaining detailed records of continuing education, policy updates, training initiatives, and compliance achievements is crucial not only for recertification purposes but also for professional credibility. Proper documentation demonstrates accountability and transparency, providing verifiable evidence of a professional’s ongoing dedication to excellence. In regulatory audits or professional evaluations, such records stand as tangible proof of diligence and competence.
As the healthcare industry continues to evolve, the Certified HIPAA Professional’s role will expand beyond regulatory enforcement to include advocacy for ethical innovation. Those who maintain their certification proactively are better positioned to influence institutional policy, shape industry standards, and mentor future compliance leaders. Their voices contribute to a collective movement that values both technological progress and the inviolability of patient privacy.
Conclusion
Sustaining CHP certification is a journey that reflects intellectual discipline, ethical fortitude, and professional adaptability. It is an enduring pledge to remain informed, competent, and principled amid an ever-changing healthcare environment. Certified HIPAA Professionals who commit to continuous education, technological literacy, and ethical consistency fortify not only their own careers but also the integrity of the institutions they serve. Their vigilance ensures that as healthcare embraces innovation, it does not compromise its moral compass. In essence, maintaining certification is not an end in itself but an evolving covenant between the professional, the law, and humanity—a testament to the timeless ideal that safeguarding privacy is integral to preserving dignity in healthcare.
Frequently Asked Questions
How can I get the products after purchase?
All products are available for download immediately from your Member's Area. Once you have made the payment, you will be transferred to Member's Area where you can login and download the products you have purchased to your computer.
How long can I use my product? Will it be valid forever?
Test-King products have a validity of 90 days from the date of purchase. This means that any updates to the products, including but not limited to new questions, or updates and changes by our editing team, will be automatically downloaded on to computer to make sure that you get latest exam prep materials during those 90 days.
Can I renew my product if when it's expired?
Yes, when the 90 days of your product validity are over, you have the option of renewing your expired products with a 30% discount. This can be done in your Member's Area.
Please note that you will not be able to use the product after it has expired if you don't renew it.
How often are the questions updated?
We always try to provide the latest pool of questions, Updates in the questions depend on the changes in actual pool of questions by different vendors. As soon as we know about the change in the exam question pool we try our best to update the products as fast as possible.
How many computers I can download Test-King software on?
You can download the Test-King products on the maximum number of 2 (two) computers or devices. If you need to use the software on more than two machines, you can purchase this option separately. Please email support@test-king.com if you need to use more than 5 (five) computers.
What is a PDF Version?
PDF Version is a pdf document of Questions & Answers product. The document file has standart .pdf format, which can be easily read by any pdf reader application like Adobe Acrobat Reader, Foxit Reader, OpenOffice, Google Docs and many others.
Can I purchase PDF Version without the Testing Engine?
PDF Version cannot be purchased separately. It is only available as an add-on to main Question & Answer Testing Engine product.
What operating systems are supported by your Testing Engine software?
Our testing engine is supported by Windows. Andriod and IOS software is currently under development.


