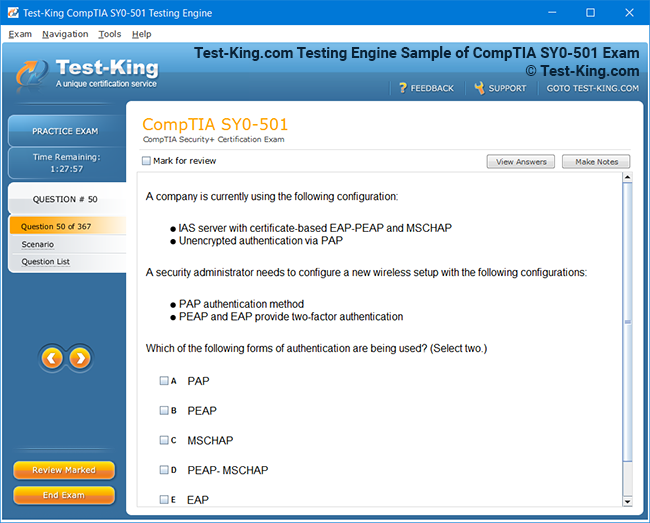
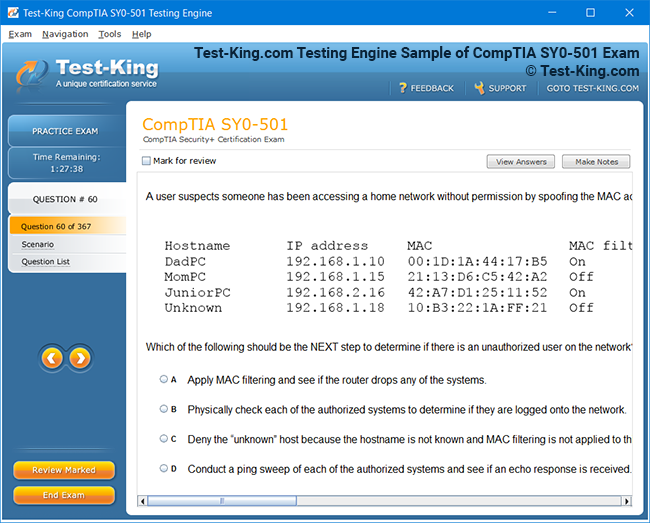
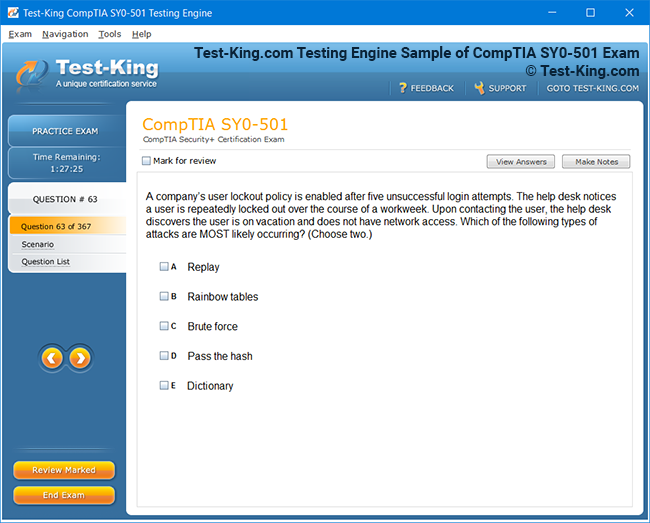
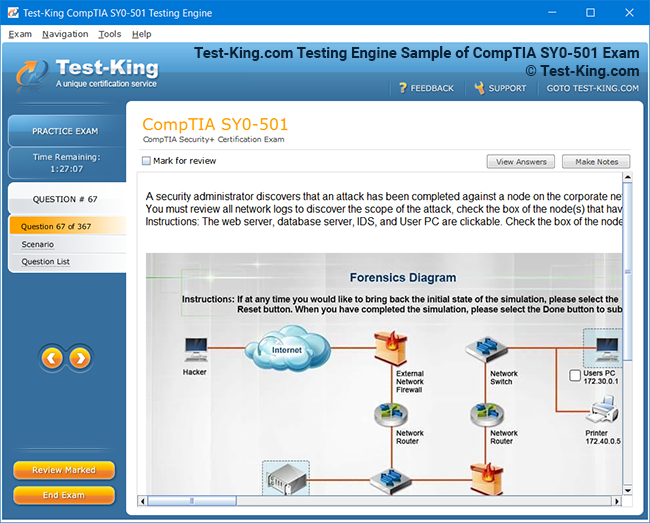
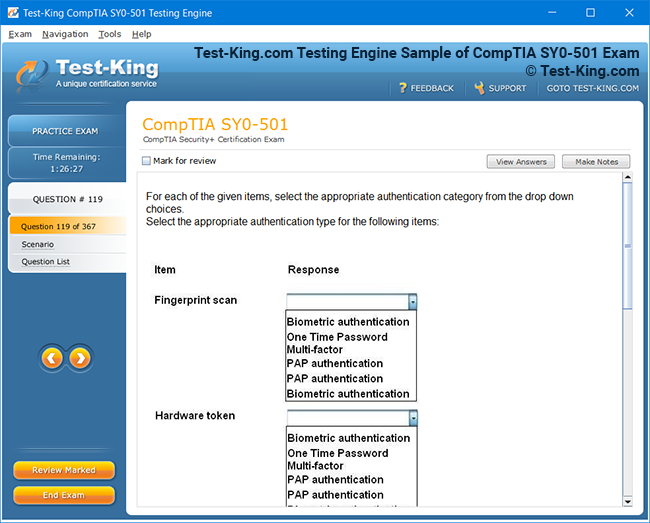
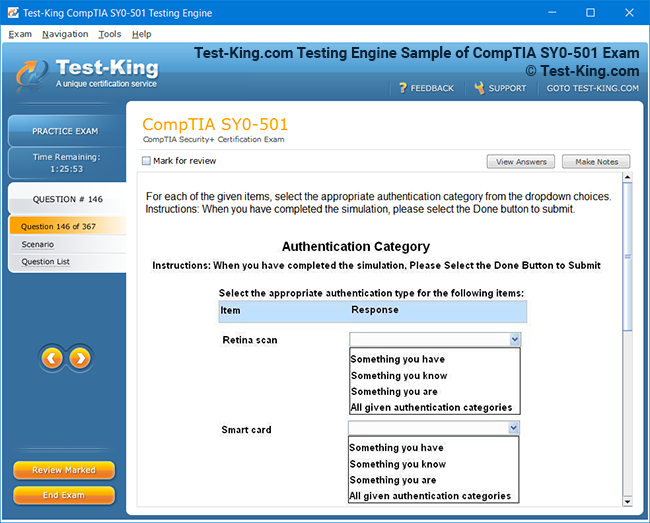
Product Screenshots
Frequently Asked Questions
How can I get the products after purchase?
All products are available for download immediately from your Member's Area. Once you have made the payment, you will be transferred to Member's Area where you can login and download the products you have purchased to your computer.
How long can I use my product? Will it be valid forever?
Test-King products have a validity of 90 days from the date of purchase. This means that any updates to the products, including but not limited to new questions, or updates and changes by our editing team, will be automatically downloaded on to computer to make sure that you get latest exam prep materials during those 90 days.
Can I renew my product if when it's expired?
Yes, when the 90 days of your product validity are over, you have the option of renewing your expired products with a 30% discount. This can be done in your Member's Area.
Please note that you will not be able to use the product after it has expired if you don't renew it.
How often are the questions updated?
We always try to provide the latest pool of questions, Updates in the questions depend on the changes in actual pool of questions by different vendors. As soon as we know about the change in the exam question pool we try our best to update the products as fast as possible.
How many computers I can download Test-King software on?
You can download the Test-King products on the maximum number of 2 (two) computers or devices. If you need to use the software on more than two machines, you can purchase this option separately. Please email support@test-king.com if you need to use more than 5 (five) computers.
What is a PDF Version?
PDF Version is a pdf document of Questions & Answers product. The document file has standart .pdf format, which can be easily read by any pdf reader application like Adobe Acrobat Reader, Foxit Reader, OpenOffice, Google Docs and many others.
Can I purchase PDF Version without the Testing Engine?
PDF Version cannot be purchased separately. It is only available as an add-on to main Question & Answer Testing Engine product.
What operating systems are supported by your Testing Engine software?
Our testing engine is supported by Windows. Andriod and IOS software is currently under development.
Top AHIP Exams
A Comprehensive Guide to the AHIP AHM-510 Exam: Mastering Governance and Regulation in Healthcare
Healthcare governance is a multifaceted discipline that underpins the operational and strategic frameworks of healthcare organizations. It encompasses the policies, procedures, and ethical standards that ensure institutions operate with transparency, accountability, and adherence to legal mandates. For professionals pursuing the AHIP AHM-510 exam, a profound comprehension of governance principles is indispensable, as it forms the backbone of compliance and regulatory practices. Governance is not merely a bureaucratic framework; it is an orchestration of decision-making hierarchies, risk mitigation strategies, and ethical stewardship designed to safeguard patient welfare, organizational integrity, and stakeholder trust.
Understanding the Foundations of Healthcare Governance and Regulation
Regulation in healthcare functions as both a guiding compass and a protective mechanism. It establishes the boundaries within which healthcare providers must operate, ensuring the delivery of quality care while mitigating potential harm. The regulatory landscape comprises federal and state statutes, accreditation standards, and policy directives that collectively shape organizational conduct. Professionals preparing for the AHIP AHM-510 exam must internalize these frameworks, as the assessment evaluates the ability to navigate complex regulatory environments and implement compliance strategies effectively.
Compliance extends beyond mere adherence to statutory requirements; it embodies a culture of ethical mindfulness and proactive risk management. An organization that fosters compliance does not only react to external audits or inspections but anticipates regulatory shifts and integrates best practices into its operational ethos. The AHM-510 exam evaluates candidates on their capacity to harmonize governance, regulation, and compliance into a coherent organizational strategy that ensures both legal conformity and ethical rectitude.
The Structure and Content of the AHM-510 Examination
The AHIP AHM-510 exam is meticulously designed to assess a candidate’s mastery of governance and regulatory principles as they apply to healthcare organizations. Its content spans multiple domains, each focusing on distinct yet interrelated aspects of organizational oversight. A primary domain addresses the foundations of healthcare governance, exploring the roles of boards, committees, and executives in shaping policy, enforcing accountability, and fostering strategic vision. Candidates are expected to comprehend not only the formal structures of governance but also the subtle dynamics of leadership, communication, and organizational culture that influence decision-making.
Another critical domain pertains to regulatory compliance, encompassing federal statutes such as the Health Insurance Portability and Accountability Act (HIPAA), the Affordable Care Act (ACA), and relevant state-specific laws. Candidates must demonstrate proficiency in interpreting these regulations, understanding their practical implications, and designing systems to ensure adherence. This includes knowledge of reporting obligations, auditing procedures, and mechanisms to address non-compliance effectively. The exam also evaluates awareness of regulatory agencies’ roles, including the Centers for Medicare & Medicaid Services (CMS), state departments of health, and accreditation organizations, emphasizing their impact on organizational operations.
Risk management constitutes an essential component of the examination. Healthcare institutions operate in environments replete with clinical, operational, financial, and reputational risks. The AHM-510 exam assesses candidates’ ability to identify potential hazards, implement mitigation strategies, and establish monitoring mechanisms that safeguard the institution. This involves understanding risk assessment frameworks, incident reporting protocols, and continuous quality improvement methodologies that collectively reduce vulnerability and enhance resilience.
Ethics, though often intertwined with governance, merits distinct attention in the examination. Ethical principles in healthcare extend beyond compliance with law and policy; they involve moral discernment in patient care, resource allocation, and organizational decision-making. The AHM-510 exam evaluates the candidate’s ability to navigate ethical dilemmas, balance competing interests, and implement policies that reflect both legal obligations and moral responsibility.
Key Competencies Assessed in the Examination
Success in the AHM-510 exam requires a combination of cognitive, analytical, and practical competencies. Analytical acumen is vital, as candidates must interpret regulatory texts, assess organizational policies, and propose solutions that reconcile operational efficiency with compliance imperatives. Critical thinking is similarly essential, enabling candidates to evaluate complex scenarios, anticipate the consequences of administrative decisions, and identify gaps in governance structures.
Communication skills are another significant area of assessment. Governance and regulation are not solely technical disciplines; they are relational, requiring effective interaction with diverse stakeholders, including board members, clinical leaders, regulatory authorities, and patients. The ability to articulate policy interpretations, explain regulatory requirements, and foster a culture of accountability is evaluated both theoretically and through scenario-based questions.
Strategic planning competencies are emphasized as well. Candidates must understand how governance frameworks and regulatory policies intersect with organizational objectives. This includes the design of compliance programs, integration of risk management processes into operational workflows, and alignment of ethical standards with strategic initiatives. Mastery in this domain reflects a professional’s ability to translate regulatory knowledge into tangible organizational benefits, ensuring sustainability, accountability, and patient-centered outcomes.
Exam Preparation Strategies and Study Approaches
Preparation for the AHM-510 exam necessitates a structured, methodical approach. Familiarity with core governance and regulatory concepts is foundational; candidates should cultivate a deep understanding of policy frameworks, compliance mandates, and ethical standards. This can be achieved through comprehensive study of federal and state statutes, organizational case studies, and best practice guidelines published by reputable healthcare institutions.
Active engagement with practice scenarios and real-world examples enhances comprehension. Exam questions often present complex situations that require integration of multiple domains, such as assessing a hospital’s response to a compliance breach or evaluating the effectiveness of a governance committee. By simulating these scenarios, candidates develop the analytical agility and decision-making proficiency required for success.
Regular review and reinforcement are crucial. The volume of regulatory content can be daunting, and retention is facilitated by organizing material thematically, summarizing key points, and employing mnemonic techniques to internalize critical frameworks. Peer discussions and study groups can also provide diverse perspectives and illuminate nuanced interpretations of governance and compliance issues.
Time management is an additional consideration. The examination tests both knowledge and the ability to apply it efficiently under timed conditions. Candidates should practice pacing, familiarize themselves with question formats, and develop strategies for prioritizing complex scenarios while avoiding pitfalls associated with misinterpretation or overanalysis.
Common Challenges and How to Address Them
Many candidates encounter challenges when preparing for the AHM-510 exam, particularly in bridging theoretical knowledge with practical application. One common difficulty is the abstraction of governance principles; candidates may understand policies in isolation but struggle to envision their operationalization. Addressing this requires a focus on case-based learning, where abstract principles are translated into actionable strategies, such as designing compliance workflows or establishing reporting hierarchies.
Another challenge lies in the voluminous regulatory content. Laws, guidelines, and agency requirements are extensive and continually evolving. Maintaining current knowledge demands disciplined monitoring of updates, subscribing to regulatory bulletins, and integrating new directives into existing mental frameworks. Understanding the interrelation between federal, state, and institutional regulations is essential to avoid errors and ensure comprehensive compliance.
Ethical decision-making can also present difficulties, particularly when regulations provide ambiguous guidance or when competing priorities create moral tension. Developing ethical reasoning skills involves studying historical case precedents, exploring frameworks such as principlism and consequentialism, and practicing scenario-based judgments that weigh legal, clinical, and organizational factors simultaneously.
Risk management challenges often involve assessing probability versus impact and prioritizing interventions accordingly. Candidates should familiarize themselves with risk matrices, mitigation strategies, and monitoring tools that translate abstract risk concepts into practical organizational safeguards. This approach ensures that governance and compliance decisions are both defensible and operationally effective.
The Significance of the AHIP AHM-510 Certification
Achieving the AHIP AHM-510 certification signifies more than the successful completion of an examination; it represents the attainment of specialized expertise in healthcare governance and regulation. Certified professionals are recognized for their proficiency in interpreting complex legal frameworks, designing compliant organizational systems, and implementing risk management and ethical strategies. This credential enhances professional credibility, opens avenues for career advancement, and demonstrates a commitment to excellence in healthcare administration.
Organizations benefit from employing professionals with AHM-510 certification, as they contribute to a culture of accountability, transparency, and continuous improvement. Certified individuals are equipped to guide institutions through audits, regulatory inspections, and policy development, thereby minimizing legal exposure and fostering operational resilience. In an environment where healthcare governance is increasingly scrutinized, the value of such expertise cannot be overstated.
Moreover, the certification encourages ongoing professional development. Governance and regulation are dynamic fields; laws change, best practices evolve, and ethical standards are continuously refined. The AHM-510 credential underscores the importance of lifelong learning and positions professionals to remain at the forefront of healthcare administration innovation.
Navigating Regulatory Frameworks and Compliance in Healthcare Organizations
Healthcare organizations operate in a labyrinthine regulatory landscape, where federal and state mandates converge with accreditation standards to shape operational, clinical, and administrative practices. Mastery of these frameworks is pivotal for professionals aiming to excel in governance and regulatory roles, particularly for those preparing for the AHIP AHM-510 exam. Regulations not only define permissible actions but also establish expectations for transparency, accountability, and ethical stewardship. An in-depth understanding of regulatory statutes, compliance obligations, and monitoring mechanisms forms the bedrock of effective governance, ensuring that healthcare institutions remain resilient, lawful, and patient-centered.
Federal statutes such as the Health Insurance Portability and Accountability Act and the Affordable Care Act delineate the parameters within which organizations must manage patient information, billing practices, and service delivery. Understanding these laws requires more than rote memorization; it necessitates an appreciation for the underlying rationale that prioritizes patient protection, equitable access, and operational integrity. Candidates for the AHM-510 exam must be adept at translating these statutory frameworks into actionable policies and procedures, ensuring that compliance is woven seamlessly into organizational workflows.
State-specific regulations add a layer of complexity, as healthcare governance and compliance often vary depending on jurisdictional requirements. Professionals must discern subtle differences in licensing mandates, reporting obligations, and quality metrics, aligning institutional practices with both state and federal standards. Regulatory agencies, including departments of health and other oversight bodies, often issue guidance documents and updates that demand continuous vigilance. Being conversant with these regulatory instruments allows administrators to preempt violations, implement corrective measures, and maintain institutional credibility.
Accreditation organizations, such as The Joint Commission, play an equally significant role in shaping governance expectations. These entities establish benchmarks for quality, safety, and operational efficacy, which extend beyond mere compliance with law. Accreditation is both a recognition of excellence and a safeguard against systemic deficiencies, emphasizing the importance of ongoing monitoring, auditing, and continuous improvement. Professionals pursuing AHM-510 certification are expected to understand how to integrate accreditation standards into the broader regulatory framework, enhancing both compliance and institutional reputation.
Compliance programs within healthcare organizations serve as the operational manifestation of regulatory understanding. These programs typically encompass policies, training initiatives, monitoring systems, and reporting mechanisms that collectively foster a culture of adherence and accountability. Designing effective compliance frameworks requires strategic insight, as policies must balance regulatory mandates with organizational efficiency and resource allocation. The AHM-510 exam evaluates candidates’ ability to construct and assess these programs, ensuring that institutional practices not only meet statutory requirements but also anticipate evolving regulatory expectations.
Risk Management and Ethical Oversight in Healthcare Governance
Risk management constitutes an essential pillar of governance, as healthcare organizations face multifaceted threats spanning clinical, financial, operational, and reputational domains. Effective risk management involves systematic identification, assessment, and mitigation of potential hazards, guided by principles that prioritize patient safety and organizational resilience. The AHIP AHM-510 exam challenges candidates to demonstrate proficiency in establishing risk assessment frameworks, implementing monitoring protocols, and devising contingency strategies that safeguard both stakeholders and institutional interests.
Clinical risks, including medical errors, patient safety incidents, and adverse outcomes, require meticulous oversight and proactive interventions. Governance structures, such as quality committees and risk management offices, serve to identify vulnerabilities, analyze causative factors, and implement corrective actions. Candidates must understand the interplay between regulatory expectations, clinical protocols, and organizational accountability, ensuring that risk management strategies are both legally defensible and ethically sound.
Operational and financial risks, encompassing inefficiencies, budgetary constraints, and resource allocation challenges, necessitate strategic foresight. Governance professionals must evaluate operational workflows, identify potential bottlenecks, and implement process improvements that align with compliance and regulatory mandates. Financial oversight includes monitoring billing practices, safeguarding against fraud, and ensuring adherence to reimbursement regulations. AHM-510 examinees are expected to synthesize these considerations, designing governance frameworks that preempt operational disruptions while enhancing organizational efficacy.
Ethical oversight is inextricably linked with risk management and regulatory compliance. Healthcare governance requires the capacity to navigate complex moral landscapes, where competing interests and ambiguous directives may challenge conventional decision-making. Ethical principles guide administrators in balancing patient rights, organizational priorities, and legal obligations, fostering decisions that reflect both integrity and prudence. For instance, allocating scarce resources, addressing conflicts of interest, or implementing disciplinary actions demands both adherence to policy and consideration of broader ethical implications. Mastery of these principles is a core competency assessed in the AHM-510 examination.
Governance Structures and Leadership Responsibilities
Understanding governance structures is fundamental for aspiring AHM-510 candidates. Boards of directors, executive leadership, and specialized committees collectively define policy direction, enforce compliance, and oversee risk management processes. Each entity has specific roles, yet effective governance relies on cohesive interaction, communication, and shared accountability. Boards, for example, are responsible for strategic oversight, financial stewardship, and ensuring regulatory compliance, while executive teams operationalize policies and manage day-to-day institutional functions. Committees, including quality assurance, ethics, and risk management committees, provide specialized guidance and monitoring, bridging the gap between strategy and practice.
Leadership responsibilities in governance extend beyond formal authority, encompassing the capacity to cultivate a culture of compliance, transparency, and ethical conduct. Leaders must communicate expectations clearly, reinforce accountability, and model behavior that aligns with organizational values. The AHM-510 exam assesses the ability to evaluate leadership effectiveness, identify structural weaknesses, and recommend improvements that enhance institutional governance. Candidates must recognize that leadership is not merely directive but relational, influencing culture, morale, and stakeholder trust.
Effective governance also involves integrating performance metrics and continuous evaluation mechanisms. Institutions must monitor policy adherence, track compliance outcomes, and adjust strategies in response to identified deficiencies. This iterative process ensures that governance remains adaptive, evidence-informed, and aligned with both regulatory requirements and institutional objectives. Professionals pursuing AHM-510 certification are expected to demonstrate the capacity to implement these systems, ensuring sustainable compliance and resilient operational performance.
Integrating Policy Development with Organizational Objectives
Policy development is a critical component of healthcare governance, linking regulatory expectations with organizational goals. Policies translate statutory requirements into actionable practices, providing clarity and direction for staff, executives, and stakeholders. Developing effective policies requires comprehensive understanding of applicable laws, ethical principles, and operational realities, ensuring that directives are practical, enforceable, and aligned with strategic priorities.
Candidates must be adept at conducting policy audits, identifying gaps, and updating guidelines in response to evolving regulations or organizational needs. Policies may address a broad spectrum of issues, including patient privacy, clinical protocols, resource allocation, and conflict-of-interest management. Each policy must harmonize legal compliance, ethical considerations, and operational feasibility, reinforcing the institution’s commitment to quality and accountability.
Integration of policy development with organizational objectives also entails performance monitoring and evaluation. Key performance indicators, reporting mechanisms, and review cycles enable institutions to measure adherence, identify trends, and implement corrective actions. For AHM-510 examinees, understanding the interplay between policy, regulation, and governance is crucial, as it demonstrates the capacity to translate theoretical knowledge into practical organizational impact.
Scenario-Based Application of Governance and Regulation Knowledge
A distinguishing feature of the AHIP AHM-510 exam is its emphasis on scenario-based evaluation, which tests the ability to apply knowledge to complex, real-world situations. Candidates may be presented with cases involving compliance breaches, ethical dilemmas, or operational failures, requiring integration of governance principles, regulatory understanding, and risk management strategies. For instance, a scenario might involve a hospital facing allegations of improper billing practices. The candidate must analyze regulatory requirements, assess organizational policies, identify responsible parties, and recommend corrective actions that ensure compliance, mitigate risk, and preserve institutional integrity.
Scenario-based questions underscore the importance of critical thinking, analytical rigor, and ethical judgment. They also illustrate the interconnectedness of governance domains: decisions in one area, such as finance or compliance, often have implications for clinical quality, patient safety, and organizational reputation. Preparing for these scenarios involves not only studying regulatory texts but also engaging in case analyses, simulations, and reflective exercises that cultivate practical problem-solving skills.
Building a Culture of Compliance and Ethical Awareness
Healthcare organizations thrive when compliance and ethics are embedded into institutional culture. Leaders and governance professionals play a pivotal role in fostering an environment where adherence to laws, regulations, and ethical standards is a collective responsibility. This involves continuous education, transparent communication, and reinforcement of policies at every level of the organization.
Training programs, workshops, and awareness campaigns equip staff with knowledge and skills to navigate complex regulatory landscapes. Open channels for reporting concerns, coupled with non-retaliation policies, encourage proactive identification of potential issues. Leaders must also recognize and reward ethical behavior, cultivating an organizational ethos where integrity is valued alongside operational performance.
For AHM-510 candidates, understanding cultural dimensions of compliance is as important as technical proficiency. A comprehensive approach integrates regulatory knowledge, governance frameworks, risk management strategies, and ethical principles into a cohesive culture that supports accountability, minimizes vulnerability, and ensures sustainable excellence in healthcare delivery.
Audit Processes and Monitoring Mechanisms in Healthcare Governance
Healthcare governance demands vigilant oversight, with audit processes serving as a fundamental instrument for ensuring compliance, transparency, and operational integrity. Auditing encompasses systematic examination of organizational policies, procedures, and activities to determine whether they conform to regulatory requirements, ethical standards, and institutional objectives. For professionals preparing for the AHIP AHM-510 exam, an in-depth understanding of audit principles, methodologies, and application in healthcare environments is essential.
Audits can be internal or external. Internal audits are conducted by organizational staff or dedicated compliance units to continuously monitor adherence to policies, detect anomalies, and recommend corrective actions. They provide real-time insights into the efficacy of governance and risk management frameworks. External audits, performed by regulatory bodies, accreditation organizations, or third-party consultants, assess institutional compliance with legal statutes, industry standards, and contractual obligations. Candidates are expected to comprehend how both audit types contribute to the institutional culture of accountability and proactive risk mitigation.
The auditing process involves multiple stages, beginning with planning and risk assessment. Professionals must identify areas with heightened vulnerability, determine audit scope, and establish criteria based on regulatory standards and organizational objectives. Data collection follows, encompassing financial records, operational reports, clinical documentation, and personnel activities. Candidates for the AHM-510 examination should be capable of evaluating this data critically, identifying patterns that suggest compliance gaps or inefficiencies, and proposing actionable recommendations.
Reporting is a critical phase in auditing. Findings must be documented meticulously, communicated to relevant stakeholders, and incorporated into governance decision-making processes. Effective reporting ensures transparency, informs risk mitigation strategies, and strengthens regulatory adherence. The AHM-510 exam evaluates the candidate’s ability to interpret audit outcomes, prioritize interventions, and implement sustainable improvements that reinforce governance structures.
Regulatory Updates and Evolving Standards
Healthcare governance operates in a dynamic regulatory landscape where statutes, guidelines, and accreditation standards continually evolve. Professionals must maintain a comprehensive awareness of changes to anticipate compliance implications and adapt institutional policies accordingly. The AHIP AHM-510 exam emphasizes the capacity to track regulatory developments, interpret their significance, and integrate new requirements into organizational workflows.
Federal updates, including amendments to HIPAA, the Affordable Care Act, and CMS directives, frequently alter compliance expectations. Professionals must discern the practical implications of these changes, evaluating how they affect patient privacy, billing practices, clinical documentation, and operational reporting. State regulations add another layer of complexity, requiring vigilance to ensure that local requirements are harmonized with federal mandates.
Accreditation bodies similarly evolve standards in response to industry trends, technological advancements, and patient safety concerns. Understanding the rationale behind these updates enables governance professionals to implement best practices, enhance quality of care, and maintain institutional credibility. Candidates must appreciate that regulatory compliance is not a static objective but an ongoing process requiring continual learning, adaptability, and strategic foresight.
Quality Improvement and Performance Enhancement
Governance and regulation are intrinsically linked to organizational quality improvement. Monitoring and enhancing performance is essential for ensuring patient safety, operational efficiency, and regulatory adherence. Professionals preparing for the AHM-510 exam must grasp how governance structures facilitate continuous improvement initiatives, integrating regulatory knowledge, risk management, and ethical oversight into performance enhancement strategies.
Quality improvement involves systematic assessment of clinical processes, administrative workflows, and patient outcomes. Data-driven methodologies, such as root cause analysis, incident review, and outcome measurement, enable institutions to identify deficiencies and implement corrective measures. Governance professionals oversee these initiatives, ensuring alignment with organizational policies, regulatory mandates, and ethical principles.
Performance metrics play a pivotal role in quality enhancement. Indicators may include patient satisfaction, clinical error rates, compliance with reporting requirements, and financial efficiency. Professionals must understand how to analyze these metrics, identify trends, and design interventions that promote both operational excellence and regulatory adherence. The AHM-510 exam tests candidates on their ability to connect governance oversight with measurable improvements, demonstrating the practical application of regulatory knowledge in real-world contexts.
Incident Management and Corrective Action
Incident management is a cornerstone of effective governance, encompassing the identification, investigation, and resolution of events that compromise compliance, patient safety, or organizational integrity. Professionals must establish clear reporting channels, investigation protocols, and corrective action plans to address issues promptly and effectively. For candidates of the AHIP AHM-510 exam, understanding incident management frameworks and their integration with regulatory requirements is crucial.
Corrective actions may include policy revision, staff retraining, process modification, or disciplinary measures. The objective is not merely to remediate individual incidents but to prevent recurrence, mitigate risk, and reinforce a culture of accountability. Professionals must balance legal obligations, ethical considerations, and operational feasibility when designing and implementing corrective measures.
Effective incident management also relies on documentation and communication. Thorough records ensure transparency, support regulatory reporting, and provide evidence of proactive governance. Sharing lessons learned across departments fosters organizational learning and continuous improvement, reinforcing compliance culture and strengthening institutional resilience.
Strategic Integration of Compliance and Risk Management
Compliance and risk management are not isolated functions; they intersect to form a cohesive governance strategy that ensures legal adherence, ethical conduct, and organizational sustainability. Strategic integration involves aligning regulatory mandates, operational objectives, and risk mitigation processes, creating a framework that supports informed decision-making and proactive oversight.
Risk assessment is a foundational component, requiring identification of potential vulnerabilities, evaluation of probability and impact, and prioritization of interventions. Compliance strategies translate regulatory requirements into practical procedures, policies, and training initiatives that reduce exposure to legal or ethical infractions. Governance professionals must ensure that these elements are interconnected, allowing the organization to respond to emerging challenges effectively.
For example, a hospital may face financial risk due to billing inaccuracies, clinical risk from patient safety incidents, and reputational risk from publicized compliance failures. By integrating risk management with regulatory compliance, leadership can implement preventative measures, monitor outcomes, and establish contingency plans that minimize the likelihood and impact of adverse events. The AHIP AHM-510 exam assesses the candidate’s ability to conceptualize and operationalize such integrated frameworks.
Ethical Considerations and Moral Accountability
Ethical considerations permeate all aspects of governance and regulation, shaping decisions in clinical care, policy development, and organizational oversight. Healthcare professionals often encounter complex dilemmas where legal requirements, institutional policies, and patient welfare may not align seamlessly. Mastery of ethical reasoning is therefore central to effective governance, and the AHIP AHM-510 exam evaluates the ability to navigate such scenarios with discernment and integrity.
Candidates must understand foundational ethical principles, including beneficence, non-maleficence, autonomy, and justice, and apply them in operational contexts. Ethical oversight involves evaluating conflicts of interest, ensuring equitable resource allocation, and maintaining transparency in reporting and decision-making. By integrating ethics into governance frameworks, professionals promote trust, accountability, and sustainability in healthcare delivery.
Training and education are essential for embedding ethical awareness across the organization. Governance leaders must cultivate an environment where ethical considerations are integrated into daily decision-making, staff are empowered to raise concerns, and policies reflect moral as well as regulatory standards. This cultural dimension reinforces compliance, mitigates risk, and enhances organizational credibility.
Case Analysis and Practical Application
The AHIP AHM-510 examination emphasizes practical application of knowledge through scenario-based assessment. Candidates are expected to analyze complex situations, synthesize regulatory and governance principles, and propose actionable solutions. Case analysis reinforces the interconnectedness of compliance, risk management, ethics, and operational oversight, demonstrating the practical relevance of theoretical knowledge.
For instance, a scenario might involve a sudden regulatory change affecting patient privacy standards. The candidate must evaluate current policies, assess gaps, propose procedural adjustments, and communicate necessary actions to staff and leadership. This exercise requires integration of legal understanding, ethical judgment, risk assessment, and governance acumen.
By engaging with case-based learning, candidates develop analytical agility, critical thinking, and strategic foresight. These competencies are not only essential for passing the AHM-510 exam but also for real-world governance, where decisions carry significant clinical, financial, and reputational consequences.
Leadership and Cultural Transformation in Healthcare Organizations
Effective governance extends beyond formal compliance structures; it necessitates leadership that inspires cultural transformation. Leaders play a central role in embedding regulatory adherence, ethical conduct, and risk-conscious behavior into the organizational fabric. By modeling accountability, communicating expectations clearly, and reinforcing performance standards, governance professionals influence staff behavior, operational culture, and institutional resilience.
Cultural transformation involves promoting transparency, encouraging proactive reporting, and rewarding ethical decision-making. Leaders must balance enforcement with education, ensuring that compliance is understood as an integral part of organizational identity rather than a punitive obligation. For candidates preparing for the AHM-510 exam, understanding the mechanisms of cultural change is as crucial as mastering technical regulatory knowledge, reflecting the multifaceted nature of effective healthcare governance.
Advanced Compliance Strategies and Regulatory Oversight
Healthcare organizations operate in environments of increasing complexity, where regulatory oversight and compliance demands require strategic acumen and operational dexterity. For professionals pursuing the AHIP AHM-510 exam, understanding advanced compliance strategies is paramount. Effective governance transcends basic adherence to rules; it requires anticipation of regulatory shifts, integration of best practices, and orchestration of policies that minimize institutional vulnerability while maximizing operational efficacy.
Advanced compliance strategies involve comprehensive policy development, regular monitoring, and proactive intervention. Policies must be constructed with both precision and flexibility, reflecting statutory obligations, accreditation standards, and ethical imperatives. Healthcare administrators must be capable of evaluating policy effectiveness, identifying latent deficiencies, and implementing enhancements that strengthen institutional resilience. The AHIP AHM-510 exam assesses the candidate’s ability to conceptualize and operationalize such strategies, ensuring they can guide organizations through complex regulatory landscapes.
Monitoring mechanisms are equally critical. Continuous surveillance of operational and clinical activities allows governance professionals to detect deviations from policy, identify emerging risks, and initiate corrective measures promptly. Sophisticated monitoring may include audits, performance metrics, risk indicators, and feedback systems that collectively foster a culture of compliance. Candidates must appreciate the interplay between these mechanisms and organizational outcomes, demonstrating how systematic oversight contributes to both legal conformity and ethical stewardship.
Regulatory Audits and Accreditation Processes
Regulatory audits serve as a cornerstone of healthcare governance, providing an external lens through which institutional compliance, risk management, and operational effectiveness can be evaluated. Audits may encompass financial records, clinical documentation, operational workflows, and personnel practices, assessing adherence to both statutory requirements and institutional policies. Professionals preparing for the AHM-510 examination must understand the scope, methodology, and strategic purpose of audits, recognizing that these evaluations are as much about improvement as they are about compliance verification.
Accreditation processes, conducted by recognized bodies such as The Joint Commission, further reinforce governance standards by establishing benchmarks for quality, safety, and operational excellence. Accreditation is not merely symbolic; it reflects an institution’s commitment to high standards and provides tangible metrics for continuous improvement. Candidates must grasp how accreditation interlinks with governance, compliance, and risk management, allowing organizations to enhance performance, demonstrate accountability, and mitigate potential liabilities.
Integrating audit and accreditation insights into governance frameworks requires analytical precision and strategic foresight. Professionals must interpret findings, prioritize interventions, and align corrective measures with institutional goals. The AHIP AHM-510 exam evaluates candidates on their ability to synthesize audit outcomes with regulatory knowledge, translating observations into actionable improvements that reinforce organizational integrity.
Healthcare Quality Metrics and Performance Evaluation
Quality metrics are essential instruments for governance professionals, offering quantifiable insights into organizational performance, patient outcomes, and compliance efficacy. Healthcare institutions rely on these metrics to identify trends, measure adherence to standards, and implement targeted improvements. Candidates preparing for the AHM-510 exam must understand the multifaceted nature of quality metrics, including clinical indicators, operational benchmarks, and patient satisfaction scores.
Clinical indicators assess the quality of care delivery, encompassing measures such as infection rates, readmission frequency, and adherence to clinical protocols. Operational benchmarks evaluate workflow efficiency, resource allocation, and administrative performance, highlighting areas where governance and compliance intersect with operational effectiveness. Patient satisfaction scores provide a qualitative lens, revealing perceptions of care quality, communication effectiveness, and institutional responsiveness. Professionals must integrate these diverse data sources, identifying correlations, disparities, and opportunities for enhancement.
Performance evaluation extends beyond measurement; it encompasses interpretation, corrective action, and continuous improvement. Governance leaders must ensure that data collection is accurate, comprehensive, and ethically conducted. Findings must inform policy revisions, staff training, risk mitigation strategies, and resource reallocation. The AHM-510 exam tests the candidate’s capacity to translate metric analysis into practical interventions that enhance organizational resilience, regulatory adherence, and patient-centered outcomes.
Emerging Trends in Healthcare Governance
The field of healthcare governance is dynamic, influenced by evolving regulatory expectations, technological innovation, and societal imperatives. Professionals preparing for the AHIP AHM-510 exam must stay attuned to emerging trends, recognizing their implications for compliance, risk management, and organizational strategy.
Technological advancements, including electronic health records, telemedicine platforms, and data analytics tools, have transformed governance landscapes. These technologies enhance monitoring, facilitate accurate reporting, and support evidence-based decision-making. At the same time, they introduce new risks related to data security, privacy, and system interoperability. Candidates must evaluate both the benefits and potential vulnerabilities associated with technological integration, developing governance strategies that maximize utility while safeguarding compliance.
Population health management and value-based care initiatives are reshaping regulatory priorities. Emphasis on patient outcomes, cost efficiency, and preventive care necessitates governance frameworks capable of accommodating shifting objectives. Professionals must understand how regulatory directives intersect with these models, ensuring policies, risk management practices, and quality monitoring systems are aligned with evolving standards.
Global health considerations also influence governance and regulation. International guidelines, cross-border collaborations, and pandemic preparedness protocols require organizations to adopt adaptable frameworks that respond to both local and global exigencies. The AHIP AHM-510 exam evaluates candidates’ ability to navigate these complex intersections, demonstrating foresight, analytical agility, and strategic judgment.
Risk Mitigation and Crisis Management
Risk mitigation is a core function of healthcare governance, encompassing identification, assessment, and proactive intervention across clinical, operational, financial, and reputational domains. Professionals must establish mechanisms for continuous monitoring, early detection of potential threats, and swift implementation of corrective measures. For the AHM-510 exam, candidates are expected to demonstrate the capacity to design and oversee comprehensive risk management frameworks that preserve organizational integrity and patient safety.
Crisis management represents an extension of risk mitigation, emphasizing rapid, coordinated response to unforeseen events that threaten operational continuity or regulatory compliance. Crises may include public health emergencies, financial disruptions, clinical incidents, or reputational challenges. Effective crisis management relies on preparedness plans, clear communication protocols, and decision-making hierarchies that enable swift, coordinated action. Candidates must integrate governance principles, regulatory understanding, and ethical considerations into crisis response strategies, ensuring decisions are legally defensible, ethically sound, and operationally effective.
Leadership Competencies and Organizational Culture
Leadership within healthcare governance extends beyond administrative authority; it involves cultivating a culture of accountability, ethical conduct, and compliance vigilance. Leaders influence organizational norms, reinforce standards, and model behaviors that reflect institutional values. For the AHM-510 exam, candidates must understand the nexus between leadership competencies and cultural transformation, recognizing that effective governance relies on both formal structures and relational influence.
Cultivating a compliance-oriented culture requires continuous education, transparent communication, and reinforcement of policies. Leaders must encourage proactive reporting of concerns, provide guidance on ethical dilemmas, and acknowledge adherence to standards as a valued organizational behavior. Embedding these principles into daily practice ensures that governance extends beyond formal mandates, creating an environment where ethical and regulatory considerations are integral to decision-making.
Scenario-Based Decision Making and Practical Governance
The AHIP AHM-510 examination places significant emphasis on scenario-based questions that assess practical application of governance and regulatory knowledge. Candidates may encounter complex situations involving compliance breaches, ethical conflicts, operational failures, or policy ambiguities. They are expected to analyze the context, integrate regulatory, ethical, and operational principles, and propose solutions that are pragmatic, legally compliant, and ethically sound.
Scenario-based exercises illustrate the interdependence of governance domains. Decisions in clinical, financial, or operational areas invariably impact compliance, risk management, and organizational culture. Preparing for these exercises requires engagement with real-world cases, simulation exercises, and reflective analysis that develops critical thinking, strategic judgment, and adaptive problem-solving skills. Candidates must demonstrate the ability to navigate multifaceted challenges with precision, foresight, and professional acumen.
Strategic Policy Alignment and Organizational Governance
Healthcare governance relies on the deliberate alignment of organizational policies with institutional objectives, regulatory requirements, and ethical imperatives. Professionals preparing for the AHIP AHM-510 exam must understand how policies act as the connective tissue linking compliance frameworks, operational procedures, and strategic goals. Policy alignment ensures that daily organizational activities adhere to statutory mandates while advancing quality care, patient safety, and institutional efficiency.
The formulation of policies begins with a comprehensive assessment of organizational priorities, regulatory landscapes, and potential risk exposures. Governance professionals evaluate operational workflows, identify vulnerabilities, and develop policies that mitigate risk while promoting best practices. Each policy serves as a guidepost, translating legal requirements into actionable protocols, clarifying responsibilities, and providing measurable standards for accountability. The AHM-510 examination assesses candidates’ ability to conceptualize and operationalize these alignments, demonstrating the capacity to translate regulatory knowledge into practical governance strategies.
Regular review and adaptation of policies are vital to maintaining compliance and organizational resilience. Regulations evolve, accreditation standards shift, and ethical expectations progress, necessitating continuous evaluation. Governance leaders must establish mechanisms for policy review, stakeholder engagement, and feedback integration to ensure relevance and efficacy. This iterative approach fosters institutional agility, anticipates regulatory changes, and strengthens the culture of compliance.
Legal Implications and Risk Assessment in Healthcare
Healthcare organizations are constantly navigating a complex legal environment, where lapses in compliance can result in financial penalties, reputational damage, and patient harm. Risk assessment is a pivotal component of governance, enabling institutions to identify potential legal exposures, prioritize mitigation strategies, and implement preventive measures. Candidates for the AHIP AHM-510 exam must demonstrate proficiency in assessing risks associated with clinical operations, financial transactions, privacy protections, and organizational policies.
Legal implications often intersect with operational processes. For instance, improper documentation of patient care can trigger both regulatory scrutiny and ethical concerns. Similarly, deviations from billing procedures may lead to financial liability and reputational damage. Governance professionals must anticipate such vulnerabilities and establish controls that ensure adherence to law, protect patient interests, and maintain organizational integrity. The AHM-510 exam evaluates the ability to synthesize legal understanding with practical governance interventions.
Risk assessment frameworks involve systematic identification of potential threats, evaluation of their probability and impact, and prioritization of mitigation strategies. Tools such as risk matrices, incident tracking systems, and predictive analytics enable governance professionals to allocate resources efficiently and respond proactively. By integrating these frameworks into organizational policy and practice, healthcare institutions can reduce exposure to adverse events, enhance patient safety, and strengthen regulatory compliance.
Operational Oversight and Governance Accountability
Effective governance requires meticulous oversight of operational functions, ensuring that organizational activities align with policies, regulatory expectations, and ethical standards. Governance professionals must establish monitoring mechanisms, reporting structures, and performance evaluation tools that provide clarity and accountability at all levels of the institution. For the AHIP AHM-510 exam, candidates are expected to demonstrate understanding of operational oversight as a central tenet of effective governance.
Operational oversight involves evaluating the efficiency, accuracy, and compliance of daily workflows. Leaders must identify areas of potential inefficiency, ensure adherence to clinical protocols, and verify that administrative functions comply with applicable statutes. Monitoring mechanisms may include internal audits, performance dashboards, and incident reporting systems, each contributing to a comprehensive picture of organizational performance. Governance professionals utilize these tools to detect deviations, address shortcomings, and reinforce institutional accountability.
Accountability extends beyond monitoring; it involves fostering a culture where ethical behavior, compliance adherence, and operational excellence are integral to organizational identity. Leaders must communicate expectations clearly, enforce policies consistently, and recognize adherence to standards as a valued behavior. Candidates preparing for the AHM-510 examination should understand how operational oversight and accountability interrelate, creating a cohesive governance framework that supports both regulatory compliance and strategic objectives.
Ethics and Decision-Making in Healthcare Governance
Ethical decision-making is a cornerstone of effective healthcare governance, guiding leaders through complex scenarios where competing interests, regulatory requirements, and patient welfare converge. Professionals must cultivate the ability to analyze dilemmas, weigh consequences, and implement actions that reflect both legal and moral obligations. The AHIP AHM-510 exam emphasizes the integration of ethical principles into governance, evaluating candidates on their capacity to navigate ambiguous situations with discernment and integrity.
Ethics in governance encompasses patient rights, equitable resource allocation, confidentiality, and transparency. Leaders must ensure that policies, operational practices, and strategic initiatives uphold these principles while maintaining regulatory compliance. Ethical oversight involves assessing organizational decisions for potential conflicts of interest, unintended consequences, and moral implications, reinforcing the trust of patients, staff, and external stakeholders.
Training and education are essential for embedding ethical awareness throughout an organization. Governance professionals cultivate an environment where ethical considerations are part of daily decision-making, staff are empowered to raise concerns, and policies reflect both regulatory mandates and moral responsibility. For candidates, understanding the symbiotic relationship between ethics, compliance, and governance is critical to mastering the principles assessed in the AHM-510 exam.
Crisis Preparedness and Contingency Planning
Healthcare organizations face an array of potential crises, from public health emergencies and clinical incidents to financial disruptions and reputational challenges. Governance structures must incorporate contingency planning and crisis preparedness to ensure resilience and continuity of operations. Candidates for the AHIP AHM-510 exam are expected to demonstrate proficiency in designing and overseeing crisis management frameworks that integrate regulatory compliance, risk mitigation, and ethical oversight.
Contingency planning involves identification of plausible scenarios, evaluation of potential impacts, and formulation of actionable response strategies. These strategies encompass communication protocols, chain-of-command clarifications, resource allocation plans, and operational adjustments. Governance professionals must anticipate the legal, ethical, and operational implications of crises, ensuring that response measures protect patients, staff, and institutional integrity.
Crisis preparedness also requires training and simulation exercises, fostering familiarity with response procedures and enhancing decision-making under pressure. Leaders must ensure that all stakeholders understand their roles, responsibilities, and reporting requirements during emergencies. By integrating preparedness into governance frameworks, organizations can minimize the disruptive impact of unforeseen events while maintaining compliance and ethical standards.
Integrating Technology into Governance and Compliance
Technological advancements have transformed healthcare governance, offering sophisticated tools for monitoring, reporting, and compliance management. Electronic health records, data analytics platforms, and telemedicine systems provide opportunities for enhanced oversight, improved patient care, and streamlined regulatory reporting. Candidates preparing for the AHIP AHM-510 exam must understand both the benefits and risks associated with technology integration in governance practices.
Technology facilitates real-time monitoring of clinical and operational activities, enabling governance professionals to detect deviations, analyze trends, and implement corrective measures swiftly. Data-driven insights support decision-making, inform policy development, and enhance risk management strategies. However, technological adoption also introduces potential vulnerabilities, including cybersecurity threats, privacy breaches, and system interoperability challenges. Candidates must evaluate these risks and integrate appropriate safeguards into governance frameworks.
The integration of technology requires strategic planning, staff training, and ongoing evaluation to ensure effectiveness and sustainability. Governance professionals must balance innovation with compliance, maintaining regulatory adherence while leveraging technological tools to improve operational efficiency and patient outcomes. Mastery of this integration is a critical competency for the AHIP AHM-510 examination.
Leadership Influence and Cultural Sustainability
Leadership within healthcare governance extends beyond administrative authority, shaping organizational culture, reinforcing ethical conduct, and promoting compliance vigilance. Leaders influence norms, behaviors, and attitudes, fostering an environment where governance principles are internalized and operationalized at every level. The AHIP AHM-510 exam evaluates candidates on their understanding of leadership’s role in cultivating cultural sustainability and aligning governance with organizational objectives.
Sustainable governance culture relies on continuous education, transparent communication, and consistent reinforcement of policies. Leaders must encourage proactive reporting of concerns, model ethical behavior, and recognize staff adherence to compliance standards as a valued contribution. By embedding these practices into daily operations, healthcare organizations reinforce accountability, mitigate risk, and enhance regulatory conformity. Candidates must demonstrate awareness of these dynamics and the ability to implement strategies that maintain cultural integrity and operational resilience.
Scenario-Based Analysis and Practical Application
The AHIP AHM-510 examination places strong emphasis on scenario-based questions that assess practical governance skills. Candidates are presented with complex, multifaceted situations requiring integration of regulatory knowledge, risk management strategies, ethical reasoning, and operational oversight. They must analyze context, identify priorities, and recommend actionable solutions that balance legal requirements, ethical imperatives, and organizational objectives.
Scenario-based analysis underscores the interdependence of governance domains. Decisions in one area, such as clinical operations, often affect compliance, risk management, and organizational culture. Preparing for these scenarios necessitates engagement with real-world cases, reflective exercises, and simulations that develop critical thinking, adaptive problem-solving, and strategic judgment. Mastery of scenario-based application demonstrates readiness to navigate complex governance challenges effectively, a central competency evaluated in the AHM-510 exam.
Innovative Compliance Strategies and Regulatory Foresight
Healthcare governance in contemporary settings requires the application of innovative compliance strategies, integrating foresight, analytics, and adaptive frameworks. Professionals preparing for the AHIP AHM-510 exam must demonstrate an understanding of how forward-looking governance structures anticipate regulatory changes, mitigate risk, and optimize institutional performance. Compliance is no longer merely reactive; it is proactive, informed by trends in legislation, accreditation standards, and ethical imperatives.
Innovative strategies may include the deployment of advanced data analytics to track adherence to policies, predictive modeling to anticipate areas of risk, and integration of digital dashboards for real-time compliance monitoring. These approaches provide governance professionals with actionable insights, enabling rapid interventions before regulatory breaches or operational inefficiencies manifest. The AHM-510 examination evaluates candidates on their capacity to conceptualize and implement such strategies, reflecting a comprehensive understanding of governance in dynamic healthcare environments.
Regulatory foresight involves systematic scanning of emerging laws, industry directives, and technological influences that shape compliance expectations. By analyzing patterns, anticipating future regulatory shifts, and embedding adaptive measures into organizational policies, governance professionals ensure that institutions maintain both legal conformity and operational resilience. Candidates must appreciate that foresight is not merely predictive; it is strategic, blending analytical acumen, ethical judgment, and operational understanding to preempt challenges.
Risk Management Evolution and Strategic Oversight
Risk management in healthcare governance has evolved beyond traditional mitigation practices into an integrated, strategic function. Candidates for the AHIP AHM-510 exam must understand how governance leaders identify potential clinical, operational, financial, and reputational threats, and implement comprehensive frameworks to address them. Risk assessment now encompasses continuous evaluation of performance metrics, predictive modeling, and scenario-based analysis to anticipate emergent vulnerabilities.
Strategic oversight involves prioritizing risks according to potential impact, establishing preventive controls, and ensuring alignment with regulatory and ethical standards. For instance, data security threats, evolving patient safety challenges, and operational inefficiencies require governance professionals to balance proactive monitoring with responsive corrective measures. The AHIP AHM-510 exam emphasizes the ability to integrate risk management into daily organizational practices, demonstrating that risk mitigation is both anticipatory and adaptive.
Ethical Leadership and Cultural Integration
Ethical leadership remains central to effective governance, shaping institutional culture, reinforcing compliance adherence, and fostering accountability. Leaders influence norms and behaviors through transparent decision-making, modeling ethical conduct, and cultivating an environment in which compliance is viewed as a shared responsibility rather than a regulatory imposition. The AHIP AHM-510 exam assesses candidates’ understanding of how ethical principles intersect with operational governance, risk management, and strategic oversight.
Embedding ethics into organizational culture requires continuous education, reflective practices, and open channels for raising concerns. Staff must be empowered to report potential violations, participate in ethical deliberations, and engage with institutional policies proactively. Governance leaders who integrate ethics into daily operations enhance trust, reinforce accountability, and strengthen alignment between institutional objectives and societal expectations.
Quality Assurance and Performance Optimization
Healthcare organizations rely on robust quality assurance mechanisms to monitor, evaluate, and improve performance continuously. Governance professionals play a pivotal role in designing frameworks that integrate compliance monitoring, clinical oversight, and operational evaluation. Candidates preparing for the AHM-510 examination must understand how to leverage performance metrics to inform policy development, resource allocation, and risk mitigation strategies.
Quality assurance encompasses multiple dimensions, including clinical outcomes, administrative efficiency, patient satisfaction, and regulatory adherence. By systematically collecting, analyzing, and interpreting these data, governance professionals identify trends, detect gaps, and implement targeted interventions. This process not only reinforces compliance but also drives continuous improvement, enhancing institutional reputation, patient safety, and operational resilience.
Scenario-based analysis is a critical tool in performance optimization. By simulating potential events, governance leaders can anticipate operational challenges, evaluate regulatory implications, and devise responsive strategies. This proactive approach equips organizations to respond effectively to unforeseen circumstances while maintaining high standards of care and compliance.
Crisis Preparedness and Organizational Resilience
Healthcare institutions operate in environments where crises are inevitable, ranging from clinical incidents to public health emergencies and financial disruptions. Governance frameworks must include comprehensive preparedness plans that anticipate potential challenges, define response hierarchies, and integrate regulatory and ethical considerations. Candidates for the AHIP AHM-510 exam must demonstrate mastery of crisis management principles and their practical application within healthcare governance.
Preparedness involves scenario planning, resource allocation, staff training, and establishment of communication protocols. Governance professionals ensure that each aspect of the organization is equipped to respond swiftly, minimizing risk to patients, staff, and institutional integrity. Contingency planning reinforces resilience by embedding adaptive strategies into operational procedures, ensuring that healthcare delivery continues seamlessly under adverse conditions.
Ethical considerations are integral to crisis management. Decisions regarding resource prioritization, patient care triage, and staff deployment require balancing operational imperatives with moral responsibility. Governance leaders must navigate these dilemmas with discernment, ensuring decisions are defensible, transparent, and aligned with both regulatory and ethical frameworks.
Integrating Technology into Compliance and Governance
Technological innovation has transformed healthcare governance, offering tools that enhance monitoring, streamline reporting, and support data-driven decision-making. Candidates preparing for the AHM-510 exam must understand how electronic health records, digital dashboards, predictive analytics, and telemedicine platforms can be leveraged to strengthen compliance and governance oversight.
Integration of technology facilitates real-time monitoring of clinical and operational processes, enabling governance professionals to detect deviations promptly and implement corrective measures efficiently. It also supports predictive analytics, which allows for identification of emerging risks, optimization of resource allocation, and proactive policy adjustments. Governance leaders must balance the benefits of technology with the need for cybersecurity, data privacy, and system interoperability, ensuring that digital tools augment rather than compromise compliance frameworks.
Effective integration requires strategic planning, training, and continuous evaluation. Governance professionals must ensure staff are proficient in utilizing technological tools, that systems are aligned with regulatory requirements, and that monitoring outputs are actionable. Mastery of this domain demonstrates readiness to navigate the complex intersection of technology, compliance, and governance, a core competency assessed in the AHIP AHM-510 exam.
Scenario Application and Analytical Proficiency
The AHIP AHM-510 examination emphasizes scenario-based questions designed to evaluate practical governance skills, analytical reasoning, and decision-making under complex conditions. Candidates must demonstrate the ability to analyze multifaceted situations, interpret regulatory and ethical requirements, and recommend solutions that optimize compliance, risk management, and operational effectiveness.
Scenario-based assessment highlights the interdependence of governance domains. Decisions regarding clinical operations, policy enforcement, risk mitigation, and ethical dilemmas are interconnected, requiring candidates to synthesize information, anticipate consequences, and prioritize interventions strategically. Engaging with scenario exercises develops critical thinking, adaptive problem-solving, and strategic foresight, preparing candidates for real-world governance challenges.
Leadership Influence and Institutional Sustainability
Leadership in healthcare governance extends beyond regulatory compliance, influencing organizational culture, operational efficiency, and ethical adherence. Governance leaders shape norms, reinforce accountability, and cultivate a culture where compliance, ethical conduct, and continuous improvement are integral to institutional identity. Candidates for the AHM-510 exam must demonstrate comprehension of how leadership impacts both culture and governance outcomes.
Sustainable governance is rooted in continuous education, transparent communication, and reinforcement of policies. Leaders encourage proactive reporting of concerns, model ethical behavior, and recognize adherence to standards as a valued contribution. Embedding these practices throughout the organization reinforces accountability, mitigates risk, and strengthens institutional resilience. Governance professionals who master these principles ensure that regulatory compliance, ethical conduct, and operational excellence are sustained over time.
Conclusion
Mastering governance and regulation in healthcare requires a comprehensive understanding of compliance strategies, risk management, ethical leadership, operational oversight, and technological integration. The AHIP AHM-510 exam evaluates professionals on their ability to synthesize these domains, apply knowledge to complex scenarios, and implement strategies that enhance organizational performance while maintaining regulatory and ethical standards.
Candidates must demonstrate foresight in anticipating regulatory changes, analytical acumen in evaluating operational and clinical performance, and ethical judgment in navigating multifaceted dilemmas. Continuous monitoring, scenario-based planning, and strategic policy alignment are essential to sustaining institutional integrity, patient safety, and operational efficiency.
Healthcare governance is both dynamic and multidimensional, demanding professionals who can integrate legal, ethical, operational, and technological considerations into cohesive frameworks. By mastering these competencies, candidates not only succeed in the AHM-510 examination but also contribute to the development of resilient, compliant, and ethically grounded healthcare organizations. Effective governance transforms policy into practice, oversight into accountability, and strategic vision into tangible institutional excellence, ensuring sustainable success in an ever-evolving healthcare landscape.